Monthly Archives: March 2018
What is Cervical Cancer?

The neck of the uterus, called the cervix, is lined with cells which, under ordinary circumstances, grow, divide and are replaced on an ongoing basis. This process called mitosis occurs throughout the body to ensure that the health and function of the cells, tissues and organ systems are maintained at optimal levels.
However, when cells divide, the good, the bad, and the ugly are replicated in the subsequent daughter cells. Cervical cancer results from a mutation in the cellular lining of the cervix, which spreads via mitosis to normal tissues and organs. Should this abnormal cell division go undetected and/or untreated, tumors will form and extensive spreading of the cancer (metastasis) will likely occur.
What Causes Cervical Cancer?
Most illnesses, including cancer, originate as a result of multiple factors working in concert. In the case of cervical cancer, there is no single cause. Rather, the initial cellular mutation is most likely triggered by one or a combination of conditions. Below are the primary causes of cervical cancer:
Smoking
Women who smoke are twice as likely as those who don’t to get cervical cancer.1 Smoke from tobacco products is carcinogenic and is linked to cellular mutation in the cervical lining and is a contributing cause of cervical cancer.
Age
Although cervical cancer can occur in women of any age, it occurs predominantly in women over 40 and rarely in women under 21. Therefore, advancing age may be considered a risk factor, or one of the many contributing causes of cervical cancer.
Human Papillomavirus (HPV)
A very common infection, the human papillomavirus (HPV), is a frequent precursor to abnormal cell growth (dysplasia) and is considered a primary cause of cervical cancer. Many women experience at least one HPV infection in their lifetime. Of the 100+ HPV strains, many are non-cancerous (benign), but others are known to cause cervical cancer (malignancy).
Compromised Immune System
A compromised immune system may compound the effects of the above and is considered to be a cause of cervical cancer, particularly in:2
Patients who have undergone organ transplant surgery. Immunosuppressive therapies are prescribed in order to stave off the body’s rejection of the implanted organ. Unfortunately suppressing the immune system can hinder the body’s ability to protect itself from disease.
Patients with HIV/AIDS
Patients with rare congenital syndromes that adversely affect their immune systems
Birth Control Pills
Long-term use (5+ years) of birth control pills is a contributing cause of cervical cancer. You should talk to your doctor about the pros and cons of various types of birth control for your situation.
Multiple Pregnancies
Multiple full-term pregnancies are a contributing cause of cervical cancer. No one really knows why this is, but it has been proven beyond doubt by large studies.
Diet
Diets low in fruits and vegetables are linked to an increased risk of cervical and other cancers. Also, women who are overweight are at a higher risk.
Signs and Symptoms of Cervical Cancer
Cancer of the cervix rarely exhibits early symptoms. By the time advanced cervical cancer symptoms are apparent, the cancer has likely metastasized1 – in other words, it has likely replicated and spread to other parts of the body. When they do present, symptoms of advanced cervical cancer may include:
- Any unusual discharge from the vagina
- Bleeding or spotting beyond your normal period
However, these symptoms of cervical cancer can also be indicative of many other conditions, most of them benign. Always consult your doctor for professional diagnosis of any medical condition.
Although most cervical cancer and early symptoms are seemingly invisible, there may be signs at the cellular level. These early signs are detectable via Pap tests administered in standard pelvic examinations.
Benign cells may divide abnormally and at an accelerated rate. This may sound like a symptom of cervical cancer, as described earlier, but in fact the cervical cells may be benign or precancerous.
Precancerous cells often behave like cancer cells. Indeed, they may turn into cancer cells if they are not treated. Typically, it takes several years for precancerous cells to mutate into cancer cells. So, rather than watching for symptoms of cervical cancer, your gynecologist will look for suspicious cell activity early during regular pelvic exams.
Scheduling regular pelvic exams is an important step women can take to prevent and detect cervical cancer.
PN 1002237 Rev B 01/2014
Available from: http://www.cancer.org/cancer/cervicalcancer/detailedguide/cervical-cancer-risk-factors
www.acog.org/publications/patient_education/bp163.cfm
Excessive Menstrual Bleeding

If your menstrual periods are so heavy that they affect your normal activities, you may have excessive menstrual bleeding. The medical term for periods that are very heavy, last longer than normal or both is menorrhagia. Symptoms may also include cramping, pelvic pain and anemia.
Excessive menstrual bleeding is a common condition that occurs for many reasons. Two of the most common causes are a hormone imbalance and uterine growths.
Hormone Imbalances
Your menstrual cycle is controlled by hormones, including estrogen and progesterone. When these hormones are out of balance, they can cause heavy periods or bleeding between periods. Causes of hormonal imbalances may include:
- Hormone changes in teens and in women nearing menopause
- Diabetes
- Thyroid disease
- Obesity
- Stress
- Strenuous exercise
- Anorexia (eating disorder)
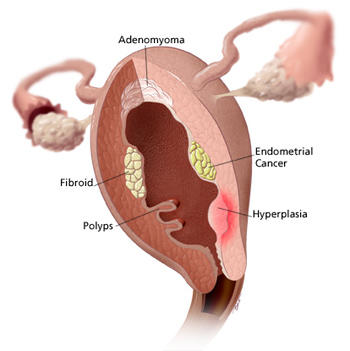
Types of Uterine Growths
- Fibroids – benign (non-cancerous) growths in or near the uterus
- Polyps – growths that attach to the inner wall of the uterus and protrude into the uterine cavity
- Adenomyosis – endometrial tissue normally lining the uterus grows into the muscular walls of the uterus
- Endometriosis – tissue that normally lines the inside of your uterus grows outside your uterus
- Endometrial cancer – an uncontrolled growth of cells in the uterine lining
- Hyperplasia – an abnormal proliferation of cells (cell division or growth) that may result in enlargement (growth) of the uterus. This term is sometimes used to refer to a benign tumor or fibroid.
Gynecology
When medicine, lifestyle changes and other non-invasive treatments cannot ease your symptoms, your doctor may recommend gynecologic surgery. Women facing gynecologic conditions such as fibroid tumors, endometriosis, heavy menstrual bleeding, cancer and pelvic prolapse often undergo surgery.

With open surgery, a large incision is made in your abdomen – large enough for your surgeon to fit his/her hands and instruments inside your body. For generations, open surgery has been the standard approach to many gynecologic procedures and is still used today. However, with open surgery there are certain drawbacks and trauma to the body due to the large incision.
There are less invasive surgical options for many women facing gynecologic surgery.
da Vinci Surgery is another minimally invasive option for women facing gynecologic surgery. With da Vinci, surgeons make just a few small incisions – similar to traditional laparoscopy. The da Vinci System features a magnified 3D high-definition vision system and special wristed instruments that bend and rotate far greater than the human wrist. As a result, da Vinci enables your surgeon to operate with enhanced vision, precision, dexterity and control.
State-of-the-art da Vinci uses the latest in surgical and robotics technologies and is beneficial for performing complex surgery. Your surgeon is 100% in control of the da Vinci System, which translates his or her hand movements into smaller, more precise movements of tiny instruments inside your body.
Endometriosis Resection
Endometriosis is when tissue that is normally in the lining of the uterus grows outside the uterus. It can be found on the ovaries, fallopian tubes, bowel and possibly other places in the pelvic cavity. Sometimes it can even grow outside the pelvis.
This extra tissue may be referred to as “implants.” During your period, the extra tissue swells with blood along with the normal tissue in your uterus. This swelling and blood can irritate nearby tissues, which can cause pain or cramps. Constant irritation may cause scar tissue known as “adhesions” to form. These adhesions can bind organs together and cause additional pain or discomfort. Adhesions may also make it difficult to get pregnant or maintain a pregnancy. In other words, adhesions caused by endometriosis can cause infertility.
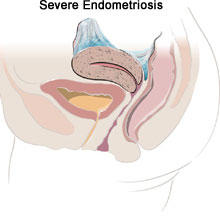
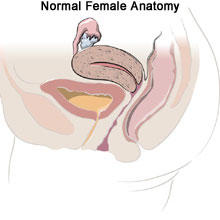
Endometriosis is one of the most common health problems for women. Symptoms are usually experienced by women in their 30s and 40s, but can occur in anyone who has menstrual periods. The exact cause of endometriosis is unknown, although there are many theories. Unfortunately, there is no cure for endometriosis but there are several treatments for the pain and infertility it may cause.
Common Symptoms of Endometriosis
If you have endometriosis, you may have one or more of these symptoms:
- Cramps and menstrual pain
- Pelvic pain
- Pain during sexual intercourse
- Infertility – trouble getting pregnant (endometriosis)
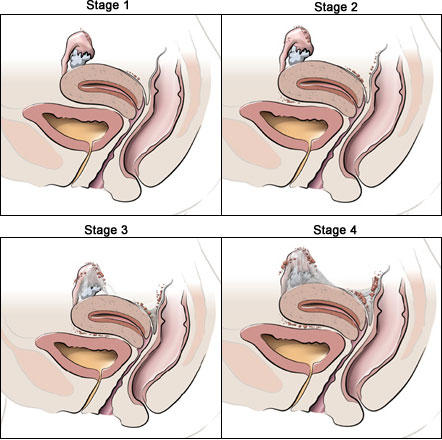
Stages of Endometriosis
The stages of endometriosis are ranked as follows: minimal (I), mild (II), moderate (III), or severe (IV). Staging of this condition depends on the number, size, and site of the implants. The stage also depends on the extent of the adhesions and whether other pelvic organs are involved. The severity of your disease may not match the pain you feel. Even mild endometriosis can cause severe pain.
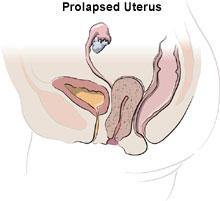
Sacrocolpopexy


The uterus is held in position by pelvic muscles, ligaments and other tissues. If the uterus drops out of its normal position, this is called prolapse. Prolapse is defined as a body part falling or slipping out of position. Prolapse happens when the pelvic muscles and connective tissues weaken. The uterus can slip to the extent that it drops partially into the vagina and creates a noticeable lump or bulge. This is called incomplete prolapse. Complete prolapse occurs when the uterus slips to such a degree that some uterine tissue is outside the vagina.
Pelvic prolapse is usually accompanied by some degree of vaginal vault prolapse. Vaginal vault prolapse occurs when the upper part of the vagina loses its shape and sags into the vaginal canal or outside the vagina. Pelvic prolapse may also involve sagging or slipping of other pelvic organs, including the bladder, the urethra which is the tube next to the vagina that allows urine to leave your body, and rectum.
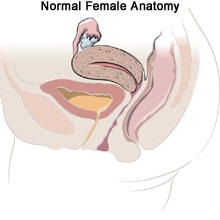
Anatomy of the Vagina
The vaginal vault is the “ceiling” or the inner, upper end of the vagina. The vaginal vault has four “compartments”: an anterior compartment, closest to the front of the body; the vaginal wall; a middle compartment consisting of the cervix; and a posterior compartment consisting of the vaginal wall at the back of the body.
Signs & Symptoms
Women with mild cases of pelvic prolapse may have no noticeable symptoms. However, as the uterus falls further out of position, it can place pressure on other pelvic organs—such as the bladder or bowel – causing a variety of symptoms, including:
- Sensation of sitting on a small ball
- Heaviness or pulling in the pelvis
- Pelvic or abdominal pain
- Pain during intercourse
- Protrusion of tissue from the opening of the vagina
- Repeated bladder infections
- Vaginal bleeding or an unusual or excessive discharge
- Constipation
- Frequent urination or an urgent need to empty your bladder
Symptoms may worsen with prolonged standing or walking due to added pressure placed on the pelvic muscles by gravity.
Causes and Risk Factors
Pelvic prolapse is fairly common and the risk of developing the condition increases with age. It can occur in women who have had one or more vaginal births. Normal aging and lack of estrogen after menopause may also cause pelvic prolapse. Chronic coughing, heavy lifting and obesity increase the pressure on the pelvic floor and may contribute to the condition. Although rare, pelvic prolapse can also be caused by a pelvic tumor. Chronic constipation and the pushing associated with it can worsen pelvic prolapse.
Screening & Diagnosis
Diagnosing pelvic prolapse requires a pelvic examination usually performed by a gynecologist. The doctor will ask about your medical history and perform a complete pelvic examination to check for signs of pelvic prolapse. You may be examined while lying down and standing. Imaging tests, such as ultrasound or magnetic resonance imaging (MRI), may be performed to further evaluate the pelvic prolapse.
Treatment
Treatment is not necessary unless the symptoms are bothersome. Most women seek treatment by the time the uterus drops to the opening of the vagina. Losing weight, stopping smoking and getting proper treatment for contributing medical problems, such as lung disease, may slow the progression of pelvic prolapse.
If you have very mild pelvic prolapse – without any symptoms – or very mild symptoms, treatment is usually unnecessary. However, keep in mind that without treatment, you may continue to lose uterine support, which could cause more severe symptoms.
Clinic Services
CLINIC SERVICES:
Obstetric Consultations:
- Infertility
- Pre-Natal Check Ups
- Care of High Risk Pregnant women
Gynecologic consultation for:
- Annual pelvic exams
- Pap smears
- Human Papillomavirus test
- Abnormal menses – irregular bleeding or prolonged or profuse bleeding
- Bleeding after sexual contact
- Abnormal vaginal discharge
- Foul-smelling vaginal discharge
- Vaginal itchiness / irritation / redness
- Sexually transmitted diseases
- Incontinence
- Urinary Tract Infections
- Pelvic tumors: myomas, polyps, ovarian cysts,
- parovarian cysts, Bartholin’s glands cysts
- Abnormal pelvic anatomy
- Vaginal growths/ lesions / tumors
- Pelvic Inflammatory Disease
- Electrocautery of warts
- IUD insertion
- Cryotherapy of Cervix
- Cancer evaluation
Others
COMPLETION CURETTAGE
A woman who has miscarried may retain some placental tissue leading to profuse or prolonged uterine bleeding and thus require a completion curettage. It is a procedure whereby a blunt instrument, a curette or curet, is inserted inside the cavity of the uterus under sedation or general anesthesia and the lining of the uterus is scraped to evacuate the products of conception.
EXPLORATORY LAPAROTOMY
This is an open surgical procedure where the abdominal or pelvic cavity is opened to inspect and/or remove diseased organs.
- Partial Hysterectomy – Removal of the uterus alone without the cervix
- Total abdominal Hysterectomy – removal of the uterus and cervix with Bilateral Salpingectomy – with removal of both Fallopian tubes or with Bilateral Salpingo-Oophorectomy – with removal of both Fallopian tubes and ovaries
Ovarian Freezing
1.Ovarian freezing sounds like a new technology. How long ago was this procedure discovered and how did it develop?
Cryopreservation is freezing tissue or cells in order to preserve it for the future. The technique of cryopreservation in reproductive medicine started with sperm freezing way back in 1953 followed by freezing of embryos in 1958. In 1986, the world’s first pregnancy using frozen eggs was reported by Dr Christopher Chen of Singapore. At that time, the fertilization rate of frozen eggs was much lower than freshly harvested eggs .


 Prior to a hysteroscopy, the patient is prepared and draped in a dorsal lithotomy position with her legs in adjustable stirrups. Care is taken to pad the pressure points to prevent any nerve impingement that may cause numbness, pain or loss of sensation.
Prior to a hysteroscopy, the patient is prepared and draped in a dorsal lithotomy position with her legs in adjustable stirrups. Care is taken to pad the pressure points to prevent any nerve impingement that may cause numbness, pain or loss of sensation.



