Monthly Archives: June 2018
First ever Robotic Pediatric Surgery in the Phil.


The first ever Pediatric Robotic Surgery was performed at the St Luke’s Global City Medical Center on June 13, 2017! This was performed on an 11 year old patient to remove an 8 cm Dermoid Cyst from the right ovary . It was full of hair, cartilage and oily sebum!! (L-R Dr Alet Hernandez, Anes, Dr Rebecca Singson, main surgeon assisted by Dr Angelica Chua and Dr Bianca Rojas w the robotic team of nurses, Kim Llanes and Berna Borneo (the latter not in the photo) .
Painless Vaginal Delivery


After a grueling day topped by a challenging robotic surgery, you’re ready to hit the sack and rest your weary body….then suddenly a mommy goes into labor since a baby boy decides to arrive on earth. In the first minute of life, he stares at you, following your voice, with his eyes wide open and with his the left pinky up (yes, his pinky finger, notice?) I completely forgot my fatigue and ended up marveling at the miracle of life I am so privileged to constantly be a part of.
Fetal Macrosomia


Mommy Pea was 5’2 with a strong family history of diabetes and so mom developed Gestational Diabetes early in pregnancy and had to be on insulin. She tried to labor without anesthesia since she was scared of epidural anesthesia. You see, Mommy Pea has slipped discs from several falls while ice skating in Japan and so she vehemently wanted to avoid any anesthesia on her spine.
As it turns labor was too painful and so she needed epidural anesthesia which, thankfully, there was no trouble inserting. But later there was no choice but to even give spinal anesthesia when the epidural started to get patchy and Mommy Pea needed an emergency C section! So much for someone who was trying to protect her spine. But thanks to expert anesthesiologists it all went well! In the end, it was no small wonder the Baby Boy Peacock couldn’t get out the normal way since he was 8 lbs 3 oz (3780g)! A Little Buddha but too HUGE a cutie for 5’2 Mommy Pea!
Cesarean section of a 27-week fetus


Cesarean section of a 27-week fetus whose mother was an extremely high risk patient with end-stage kidney failure prior to pregnancy. It was a major challenge with multi-specialty care all throughout her pregnancy. Finally, the uncontrolled hypertension made the team decide to bring out the baby by Cesarean section to a safer environment outside the mother’s womb . It was a miracle to have even brought the pregnancy this far! The baby did well and is now a healthy baby boy!
Honeymoon Cystitis
Rebecca B. Singson, M.D, FPOGS, FACS, PSCPC
WHAT IS HONEYMOON CYSTITIS?
This is actually a form of urinary tract infection which is common during the honeymoon or immediately after. Cystitis means inflammation of the bladder and it is usually due to infection. Bacteria are often pushed mechanically up the urethra and into the bladder during sexual contact. This primarily affects the woman and the symptoms are usually that of frequency of urination, burning sensation during urination or waking up more than once while asleep to urinate. Very often, it is caused by the E.coli bacteria from the anus which gets dragged towards the vagina and urethra, and finds its way through the urethra’s tube passageway to get to your bladder, thus causing infection of the bladder. Sometimes, when the infection erodes a blood capillary in the bladder, you may even see bloody urine.
The male urethra, being longer, is not usually affected. The term ‘honeymoon’ was applied because, in the past, this was expected to be the time of first intercourse, which is no longer the norm. Of course, urinary tract infection after sex occurs at many times beyond the traditional ‘honeymoon’ – from the onset of sexual activity into old age.
HOW IS IT TREATED AND HOW CAN IT BE AVOIDED?
It is, however, easily treated with a 3-day antibiotic and the symptoms can resolve within a few days. For prevention, urinate immediately after sexual contact to discourage bacteria from going up to the bladder, wash in a front to back direction to avoid contaminating the vagina and urethra with organisms coming from the anus, and never hold your urine when you feel like voiding so you don’t encourage the bad bacteria to adhere to the bladder walls and multiply.
CAN ORAL OR RECTAL SEX CAUSE URINARY TRACT INFECTION?
Yes. The most common cause of urinary tract infection in 85% of cases is E coli. E. coli can be a normal resident in the mouth.1 In 10% of cases UTI is caused by Klebsiella, Proteus, Pseudomonas and Enterobacter. Pseudomonas may or may not be found in the mouth. In less than 5% of cases, UTI can be caused by Staph aureus, enterococcus, fungi and others. Both Staph aureus and enterococcus are normal residents of the mouth.1 Having oral sex introduces these bacteria to the urethra which can creep up to the bladder and induce infection.
Rectal sex can definitely induce UTI because the rectum is ridden with E. coli. The potential is even heightened if the male, after rectal sex, performs vaginal intercourse without adequate washing.
I KEEP GETTING URINARY TRACT INFECTION EACH TIME AFTER SEXUAL CONTACT, WHAT CAN I DO?
Up to 20 percent of young women with acute cystitis develop recurrent UTIs sexual intercourse has definitely been linked to be a cause. When these episodes recur, the organism causing it should be identified by urine culture and then documented to help differentiate between relapse (infection with the same organism) and recurrence (infection with different organisms). Fortunately, most recurrent UTIs in young women are uncomplicated infections caused by different organisms. It has been found that there may be some value in taking cranberry juice or tablets
Studies show that cranberry juice can reduce bacteria levels and discourage new bacteria from taking hold in the urinary tract. (Drinking cranberry juice won’t cure an existing infection, though, so if you’re having symptoms, you still need to see your doctor immediately to get a prescription for antibiotics.)
Recommended doses range from 90 to 480 milliliters (3 to 16 ounces) of cranberry cocktail twice daily, or 15 to 30 milliliters of unsweetened 100% cranberry juice daily. 300 milliliters per day (10 ounces) of commercially available cranberry cocktail (Ocean Spray®) has been used in well-designed research.
Other forms of cranberry used include capsules, concentrate and tinctures. Between one and six 300 to 400 milligram capsules of hard gelatin concentrated cranberry juice extract, twice daily by mouth, given with water 1 hour before meals or 2 hours after meals has been used.
Honeymoon cystitis can turn a lovely honeymoon into a wretched one. Be aware of it and take measures to prevent it to keep your honeymoon memorable and not miserable.
The following tips will help you prevent UTIs:
- After a bowel movement, wash and wipe yourself in a front to back direction to prevent bacteria from the stools from contaminating the urethra. Use your forefinger and middlefinger for the vaginal area and the ring and pinky fingers for the anal area to avoid contamination.
- Wash with lactic acid based vaginal wash (not soap since it is the wrong ph for the vaginal) before intercourse and urinate immediately after intercourse to prevent the organism from ascending through the ureter to the bladder.
- Avoid douching because it mechanically removes your protective bacteria, thus, making you more prone to infections.
- Avoid feminine sprays, powders and soaps that can irritate your urethra and genitals and make them a better breeding ground for bacteria.
- Never ignore your urge to pee. Keep the urine in the bladder encourages bacterial multiplication and increases the chances of the bacteria adhering to the lining of the bladder causing infection.
- Drink plenty of water, at least eight 8-ounce glasses a day to keep urine dilute.
Pap Smears: When and How Often?
Cervical cancer is the most common cancer in the female reproductive tract and is the second most common cancer in women next to breast cancer. It is however a more deadly cancer since for every 4 Filipinas who survive breast cancer, only 2 or 3 will survive cervical cancer. In Asia, there are 266,000 new cases of cervical cancer diagnosed each year. Of these, 7225 new cases are from the Philippines alone, according to our 2005 National Cancer Institute statistics. The sad thing is that two-thirds of these cases are diagnosed at a late stage when they are beyond the operative stage such that 32.3% of them die in 1 year and 73% will die in 5 years.
In developed countries where medicine is socialized and where mass screening with Pap smears is mandated, the incidence of invasive cervical cancer has declined tremendously. This is because the disease is caught at a pre-cancerous or early stage where the disease can still be eradicated without major surgery.
WHAT IS THE PAP SMEAR?
The conventional Pap smear is most inexpensive screening test for cervical cancer. It involves taking a sample of cells from the cervix (which is the opening of the uterus) either with a brush, a spatula or a cotton swab, smearing this on a glass slide and fixing it with a solution so the Pathologist can look under the microscope for any cancerous cells or signs of infection. Conventional pap smear, however have a high failure rate, and is estimated from 50-80% accurate. A new method of Pap smear called the liquid based pap test has improved accuracy by about 54%.
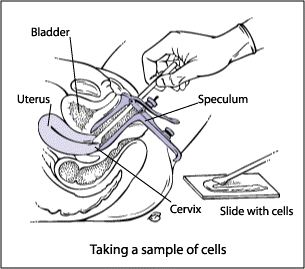
Fig 1. How to perform a Pap smear.
With the liquid-based pap test, the cells taken from the cervix are rinsed in a small vial of special solution to preserve the cells. At the laboratory a machine is able to separate the blood and mucus from the cervical cells which are then tested for abnormalities. Research shows this new method of pap test significantly increases the ability of the doctor and laboratory to identify cervical abnormalities.
WHO SHOULD HAVE A PAP SMEAR AND HOW OFTEN?
In 2016 the American Cancer Society came out with the following guidelines for early detection of cervical cancer:
- All women should start having Pap smears from age 21-29 every three years. No HPV screening is necessary.
- From age 30-65, women are recommended to test for both the Pap smear and HPV test.. If the HPV test is negative, the Pap smear and HPV can be done every 5 years. However, for women who have certain risk factors such as diethylstilbestrol (DES) exposure before birth, HIV infection, or are immunocompromised due to, chemotherapy, chronic steroid use, or organ transplant should still continue to have annual Pap smears.
- Another option for women 30-65 years old is to have only Pap smear without HPV testing every three years
- For women over 30 years old with access to a center where the Human Papillomavirus is tested may opt for HPV testing. If found to be negative, they may be defer screening to every 5 years with either the conventional or liquid-based Pap test, plus the HPV DNA test.
- Women 65 years of age or older who have had regular screening for the last 10 years 3 or more normal Pap tests in a row and no abnormal Pap test results in the last 10 years may choose to stop having cervical cancer screening. Women with a history of cervical cancer, DES exposure before birth, HIV infection or a weakened immune system should continue to have screening as long as they are in good health.
- Women with a history of CIN2 or CIN3 should continue to have testing for at least 20 years after the abnormality was found.
- Women who have had a total hysterectomy (removal of the uterus and cervix) may also choose to stop having cervical cancer screening, unless the surgery was done for treatment for cervical cancer or for a precancerous lesion. Women who have had a hysterectomy without removal of the cervix should continue to follow the guidelines.
It is always helpful to tell women to see their gynecologist for an annual check-up on their birth month so they don’t ever forget that on their birthday, their gift to themselves is their health. Having a regular check up can help you catch cervical cancer before it catches you.
Indications, Risks and Benefits
Rebecca B. Singson, MD, FPOGS, FACS, FPSGE, FPSCPC
A Cesarean section or C section is a surgical delivery of one baby or multiple babies by cutting through the mother’s abdomen and the uterine wall. If the surgery is scheduled ahead of time, it is referred to as an elective cesarean section (as opposed to an unscheduled emergency Cesarean section). There has been an increased rate of Cesarean sections recently According to Williams Obstetrics, these are the following indications for C sections:
MATERNAL INDICATIONS
Prior Cesarean delivery – because of the scar in the uterus, there is a risk of uterine rupture if the mother goes into labor after a previous Cesarean delivery although it is said to be <1%.
Abnormal placentation – this may be due to placenta previa or placenta accreta. Placenta previarefers to low implantation of the placenta. It classically presents as painless vaginal bleeding in the third trimester secondary to an abnormal placentation near or covering the internal cervical os.
Placenta accreta is when the placentagrows too deeply into the uterine wall.It can cause massive bleeding usually after delivery, since the placenta fails to detach.
Maternal request – a mother may elect to deliver by C section before or after going into labor even when there is no firm indication for a C section. Women who desire elective primary Cesarean delivery should be presented with the advantages and disadvatages. Although a C section may offer decreased risks for hemorrhage and chorioamnionitis compared with a planned primary vaginal birth, it does carry with it the disadvantage of higher rates of maternal thromboembolism, hysterectomy, and re-hospitalization for infection or wound complications; longer initial hospital stays; and higher chances of uterine rupture or abnormal placental implantation in subsequent pregnancies.3,4,5 Women who undergo a Cesarean delivery are much more likely to be delivered by a repeat operation in subsequent pregnancies.
Another advantage of a Cesarean delivery is that it is associated with lower rates of urinary incontinence and pelvic organ or uterine prolapse.6,7,8,9,10
Prior classical hysterotomy the uterus – if there has been a previous Cesarean section where the uterus has been incised the Classical way, which means the uterus was incised in the contractile portion of the uterus, there is an indication to perform a subsequent Cesarean section. Because the risk of uterine rupture in women with prior Classical Cesarean deliveryis about 9%11 it may be prudent to schedule a repeat Cesarean deliveryat 36-37 weeks. The danger, though, is the higher risk for respiratory distress syndrome in the fetus.
Unknown uterine scar type – if a patient has undergone a previous surgery on the uterus whether for a removal of a myoma or a previous C section, or if it is unknown whether a low cervical Cesarean section or a Classical Cesarean section was performed, there is an indication to perform a repeat Cesarean section.
Uterine incision dehiscence – Cesarean section in advanced labor is associated with increased risk of incomplete healing of the uterine incision leading to uterine incision dehiscence. The reported incidence of this condition ranges between 0.2% and 4.3% of all pregnancies associated with a previous C section.12 A repeat C section is indicated to repair the thinned out uterine wall.
Prior full-thickness myomectomy – A myomectomy scars the uterus and increases the risk for uterine rupture with subsequent pregnancy if allowed to go into labor.
Genital tract obstructive mass – the presence of a myoma in the cervix, or a vaginal tumor would be some types of genital obstructive masses that would prevent a normal birth and would have to be delivered by C section.13
Invasive cervical cancer – Women with cervical cancer are better delivered by C section than by vaginal birth.The recommendation is based on the finding that women diagnosed with cervical cancer within 6 months after delivering a baby, particularly vaginally, had poorer survival and higher risk of recurrent disease than women who were diagnosed with cervical cancer during their pregnancy.
Prior trachelectomy – Patients who underwent removal of the cervix for benign or malignant reasons are better delivered by Cesarean section.
Permanent cerclage – patients with incompetent cervix with permanent cercalge to keep the cervix closed may undergo an elective C section.
Prior pelvic reconstructive surgery – there are some women, especially those with exposure to a drug called diethylstilbestrol, who develop abnormalities in their reproductive organs like a double uterus, or a uterus with a septum, etc. These can cause infertility and therefore, may need reconstruction to unify the uterus or remove the septum. In some procedures which involve cutting through the uterus to unify the two cavities, called the Strassman procedure, it will be necessary to deliver by Cesarean section to prevent the uterus from rupturing on or before labor.
Pelvic deformity – there are certain types of pelvic bones that cannot support a vaginal birth. In the past, this was validated by x-rays, called x-ray pelvimetry. But present practice guidelines no longer favor exposing the fetus to radiation but instead favoring a trial of labor and an eventual C section should labor not progress. The reason for this is that even if the x ray pelvimetry reports a contracted pelvis, but the fetus is small, the baby can still be successfully be delivered vaginally.
Herpes Simplex Virus infection – if active lesions are present at the onset of labor, a Cesarean section should be recommended to prevent the fetus from acquiring the virus.14 However, if the membranes have been ruptured for more than 6 hours, it is not certain that a Cesarean section would benefit the baby. A Cesarean section can reduce, but cannot totally eliminate, the risk of newborn infection.14,15. A recent study found that a Cesarean section delivery reduces the risk of HSV among newborns by 86%16.
Human Papilloma Virus infection – HPV DNA has been detected in amniotic fluid, placenta, and the umbilical cord.17 Both chorionic and placental tissue can be infected through the hematogenous (by blood) route and hence, HPV can be spread to amniotic cells that are then ingested by the fetus18,19. Another possible route of transmitting the HPV virus is through the placenta. The virus can possibly go up via the maternal genital tract, since it has been shown that the HPV-DNA can be present, both in amniotic fluid19 and the umbilical cord,18 in pregnant women with cervical intraepithelial lesions.
Cardiac disease – various researches bear out that women with heart disease end up with a Cesarean section more often then healthy women. 20,21 However, the fact is, in patients with cardiac problems, the preferred mode of delivery is via a vaginal birth, since a Cesarean section is associated with more blood loss and higher thromboembolic and infection risk. A Cesarean section in a woman with heart disease is reserved only for obstetric indications. Examples of situations in which primary a Cesarean section should be considered are: if a woman goes into labor while on oral anticoagulants (because of risk of fetal intracranial bleeding), Marfan syndrome with diameter of the ascending aorta >45mm, acute or chronic dissection, and acute heart failure.22
Pathology requiring concurrent intra-abdominal surgery – if a woman develops cervical or ovarian cancer that requires a hysterectomy after delivery of the baby, it is warranted to perform a CS hysterectomy.
Perimortem Cesarean delivery – In cases where the mother is dying or dies while pregnant from an accident, heart diseases or cancer, etc, the baby has to be evacuated as a life-saving measure.
MATERNAL-FETAL INDICATIONS
Cephalopelvic disproportion (CCPD)– it is a condition when a baby’s head or body is too big to fit through the mother’s pelvis. Many cases of “failure to progress” during labor are given a diagnosis of CPD. Risk factors for CPD are Estimated Fetal weight of > 3,000 g, pre-pregnancy body mass index (BMI) > or = 25 kg/m2, nulliparity (never been pregnant before) and the inadequacy of clinical pelvimetry.23
Failed operative vaginal delivery – In the past, the forceps and vacuum were used to deliver the head for the more difficult cases of cephalopelvic disproportion. As cesarean delivery became more widely available in the early to mid-20thcentury, new practices were developed to minimize morbidity and maximize safety of operative vaginal delivery.One such practice which evolved, is the concept of a trial of forceps or vacuum. This approach utilizes a double set- up such that if the forceps or vacuum fails, an immediate cesarean delivery can be done.24
Placenta previa or placental abruption – a low-lying placenta, especially if it covers part or all of the internal opening of the cervix necessitates delivery by Cesarean section. Abruptio placenta involves partial or total premature separation of the placenta while the fetus is still in the womb, thus, cutting the oxygen supply to the fetus. It is a dire, life-threatening emergency which may need immediate C section.
FETAL INDICATIONS
Non-reassuring fetal status – Late decelerations (drop in fetal heart rate below 120 beats/min), bradycardia (slowed heart rate) less than 70 beats per minute, and abnormal fetal heart rate patterns during the first stage of labor might jeopardize fetal well-being, and an expedited delivery should be considered.25
If a vaginal birth is not imminent and the forceps or vacuum cannot be used, an emergency Cesarean section should be performed.
Malpresentation – if the baby’s head is not presenting properly in the birth canal, this may result in failure of the labor to progress. This can happen when the baby is in breech (the buttocks are in the birth canal instead of the head), face, brow, and compound presentations as well as when the baby is in a transverse lie. Risk factors include multiple pregnancies, previously affected pregnancy, polyhydramnios (too much amniotic fluid, i.e., amniotic fluid index above 18), and fetal and uterine anomalies.26
Macrosomia – The term fetal macrosomia implies fetal growth beyond a specific weight, usually 4,000 g (8 lb, 13 oz) or 4,500 g (9 lb, 4 oz), regardless of the fetal gestational age.In macrosomic infants, the risk of fracture of the clavicular bone in the shoulder and brachial plexus injury is approximately 10-fold and 18- to 21-fold, respectively, when birth weight is more than 4,500 g. The risk of Cesarean delivery in women attempting a vaginal delivery at least doubles when the fetal weight is estimated to be more than 4,500 g.27
Congenital anomaly – Cesarean delivery may improve neonatal outcome for fetuses with isolated brain deformities like meningomyelocele, hydrocephalus with concomitant macrocephaly, anterior wall defects with extracorporeal liver, sacrococcygeal teratomas, hydrops, and alloimmune thrombocytopenia with low platelet count at term. Hydrocephalus without macrocephaly, anterior wall defects without an extracorporeal liver, ovarian cysts, skeletal dysplasias, fetuses whose mothers have immune thrombocytopenic purpura and fetuses with alloimmune thrombocytopenia with acceptable platelet counts may safely be delivered vaginally.28
Abnormal umbilical cord Doppler study – Fetal Doppler flow velocimetry of umbilical and middle cerebral arteries allow for finding of the most proper time of high-risk pregnancy termination, hence should be considered in the elective cesarean sections.29
Thrombocytopenia – this is a condition with low platelet count in the blood and therefore makes the mother more prone to bleeding. Thrombocytopenia is second only to anemia as the most common hematologic abnormality during pregnancy.30
Prior neonatal birth trauma – “Traumatic birth” may refer to physical injury, as well as psychological trauma. In a traumatic birth, it is found that women lose more than just their dream of birth and usually judge themselves to be inadequate in some way. A traumatic birth may arise from the mother’s perceptions in relation to the use of pitocin, forceps, vacuum extraction, and Cesarean section. It can also be related to fear of maternal or fetal death, unrelieved pain during labor and/or childbirth, long and difficult labor, perceived loss of control during the childbirth experience, and a dead or damaged infant.31
Obstetricians must recognize the potential benefits as well as risks of an elective Cesarean section among the birth options for a select group of previously traumatized pregnant women. Although, with support, many women successfully deal with their prior birth trauma, some women, even with therapy, cannot come to terms with it. Therefore it is reasonable to seriously consider their request for an elective Cesarean birth in order to prevent further trauma.32
Risks to the baby during Cesarean section include:
- Breathing problems. Several studies have documented the high incidence of respiratory distress and NICU admissions in infants born by Cesarean delivery before the onset of spontaneous labor.33,34 Babies born by scheduled C section are more likely to develop transient tachypnea — a breathing problem marked by abnormally fast breathing during the first few days after birth.
- Surgical injury.Although rare, accidental nicks to the baby’s skin on the baby’s head, face or whatever part is next to the uterus as the obstetrician is incising the uterus.
Risks to the mother during Cesarean section include:
- Infection.After a C section, the mother might be at risk of developing an infection of the lining of the uterus (endometritis). This can be caused by vaginalbacteria entering the uterus during childbirth and causinginfection within six weeks of the birth (postpartum endometritis). Postpartum endometritis occurs after about 1% to 3% of vaginal births, and up to 27% of cesarean births. Prolonged rupture of the membranes (breaking the bag of water that surrounds the baby) and multiple vaginal examinations during birth also appear to increase the risk.35
- Postpartum hemorrhage (PPH). A C section might cause heavy bleeding during and after delivery. The PPH rate in an emergency Cesarean (6.75%) was greater than after an elective Cesarean (4.84%). Risk factors for PPH after an elective operation include the presence of fibroids or leiomyomata, blood disorders, placenta previa, antepartum bleeding, preterm birth, and general anesthesia. Emergecy Cesarean PPH risk factors included blood disorders, retained placenta, antepartum transfusion, antepartum/intrapartum hemorrhage, placenta previa, general anesthesia, and macrosomia.36
- Reactions to anesthesia.Adverse reactions to any type of anesthesia are possible. Luckily, in spite of an increase in the number of Cesarean sections, the incidence of anesthetic-related complications remains low. This is due primarily to the increasing use of regional anesthesia (spinal and or epidural anesthesia). With spinal anesthesia, spinal headaches may occur, and rarely, infection on the site. General anesthesia, on the other hand, a is associated with a 17-fold increase in complications, in particular, failed endotracheal intubation, aspiration of gastric contents and hypoxia.37
- Blood clots.A C section might increase the risk of developing a blood clot inside a deep vein, especially in the legs or pelvic organs (deep vein thrombosis). If a blood clot travels to the lungs and blocks blood flow (pulmonary embolism), the damage can be life-threatening.
- Wound infection.Depending on the risk factors and whether an emergency C section is needed, one might be at increased risk of an incision infection.
- Surgical injury.Although rare, surgical injuries to the bladder or bowel can occur during a C section. If there is a surgical injury during the C-section, additional surgery might be needed.
- Increased risks during future pregnancies.After a C section, one is faced with a higher risk of potentially serious complications in a subsequent pregnancy than after a vaginal delivery. The more C sections a woman has, the higher the risks of placenta previa and a condition in which the placenta becomes abnormally attached to the wall of the uterus (placenta accreta). The risk of the uterus tearing open along the scar line from a prior C section (uterine rupture) is also higher if a VBAC is attempted.
- Cunningham FG, et al. Williams Obstetrics. 24th Ed. 2014. 587-88.
- Guise JM, McDonagh MS, Osterweil P, Nygren P, Chan BKS, Helfand M. Systematic review of the incidence and consequences
- Declercq E, Barger M, Cabral HJ, et al: Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstet Gynecol 109(3):669, 2007
- Geller EJ, Wu JM, Jannelli ML, et al: Maternal outcomes associated with planned vaginal versus planned primary cesarean delivery. Am J Perinatol 27(9):675, 2010
- Liu SL, Liston RM, Joseph KS, et al: Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ 176(4):455, 2007
- Glazener C, Elders A, Macarthur C, et al: Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG 120(2):161, 2013
- Gyhagen M, Bullarbo M, Nielsen TF, et al: The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120(2):144, 2013
- Handa VL, Blomquist JL, Knoepp LR, et al: Pelvic floor disorders 5–10 years after vaginal or cesarean childbirth. Obstet Gynecol 118(4):777, 2011
- Leijonhufvud A, Lundholm C, Cnattingius S, et al: Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol 204(1):70.e1, 2011
- Rortveit G, Daltveit AK, Hannestad YS, et al: Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med 348(10):900, 2003
- Chauhan SP1,Magann EF,Wiggs CD,Barrilleaux PS,Martin JN Jr. Pregancy after classic cesarean delivery. Obster Gynecol 2002 Nov 100(5 Pt 1):946-50.
- Baron J., Weintraub A. Y., Eshkoli T., Hershkovitz R., and Sheiner E.. 2014.The consequences of previous uterine scar dehiscence and cesarean delivery on subsequent births.Int. J. Gynaecol. Obstet.126:120–122.[PubMed]
- https://www.medscape.com/viewarticle/411928
- Stone KM, Brooks CA, Guinan ME, et al. National surveillance for neonatalHerpes simplexvirus infection.Sex Trans Dis1989;16:152-6.[PubMed]
- Whitley RJ, Corey L, Arvin A, et al. Changing presentation of neonatalHerpes simplexvirus infection.J Infect Dis1988;158:109-16.[PubMed]
- Brown ZA, Wald A, Morrows A, et al. Effect of serologic status and cesarean delivery on transmission rates ofHerpes simplexvirus from mother to infant.JAMA2003;289:203-9.[PubMed]
- Rombaldi RL, et al. Perinatal transmission of human papillomavirus DNA, Virol J, 2009, 6:83.
- Syranjen S. Current concepts on human papillomavirus in children. APMIS, 2010, 118: 494-509
- Armbruster-Moraes E, et al. Presence of human papillomavirus DNA in amniotic fluids of pregnant women with cervical lesion, Gynecol Oncol, 1994, 54:152-8.
- Yap SC, Drenthen W, Pieper PG, et al. On behalf of the ZAHARA Investigators. Risk of complications during pregnancy in women with congenital aortic stenosis.Int J Cardiol.2008;126:240–246. doi: 10.1016/j.ijcard.2007.03.134.[PubMed][Cross Ref]
- Balci A, Drenthen W, Mulder BJ, et al. Pregnancy in women with corrected tetralogy of Fallot: occurrence and predictors of adverse events.Am Heart J.2011;161:307–313. doi: 10.1016/j.ahj.2010.10.027.[PubMed][Cross Ref]
- Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C et al. ESC guidelines on the management of cardiovascular diseases during pregnancy of the European Society of Cardiology. Eur Heart J. 2011; Aug 26 (Epub ahead of print; doi:10.1093/eurheartj/ehr218)
- Surapanthapisit P1,Thitadilok W. Risk factors of caesarean section due to cephalopelvic disproportion. J Med Assoc Thai.2006 Oct;89 Suppl 4:S105-11.
- James, A, et al. Failed Operative Vaginal Delivery. Obstet Gynecol. 2009 Nov; 114(5): 1017–1022.
- Sheiner, E, et al. Clinical significance of fetal heart rate tracings during the second stage of labor. Obstet Gynecol 2001 May;97(5 Pt 1):747-52.
- Sharshiner R1,Silver RM.. Management of fetal malpresentation.
Clin Obstet Gynecol2015 Jun;58(2):246-55. doi: 10. 1097/GRF. 0000000000000103. - Chatfield, J. ACOG issues guidelines of fetal macrosomia. Am Fam Physician.2001Jul1;64(1):169-170
- Kuller JA, et al. Cesarean delivery for fetal malformations. Obstet Gynecol Surv. 1996 Jun;51(6):371-5.
- Mizgiert, et al. Fetal flow velocimetry measurements as indications for cesarean section. Ginekol Pol. 1997 Aug;68(8):337-43.
- Sullivan CA, Martin JN., Jr Management of the obstetric patient with thrombocytopenia.Clin Obstet Gynecol.1995;38:521–34.[PubMed]
- Panuthos C, Romero C. 1984.Ended beginnings: Healing childbirth losses. Westport, CT: Greenwood Publishing Corp.
- Patti Spiegelberg Gardner, CNM, MSN. Previous Traumatic Birth: An Impetus for Requested Cesarean Birth. J Perinat Educ. 2003 Winter; 12(1): 1–5. doi:10.1624/105812403X106676
- Zanardo V, Padovani E, Pittini C, et al. The influence of timing of elective cesarean section on risk of neonatal pneumothorax.J Pediatr.2007;150:252.[PubMed]
- Zanardo V, Simbi AK, Franzoi M, et al. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery.Acta Paediatr.2004;93:643.[PubMed]
- Mackeen AD, Packard RE, Ota E, Speer L.Antibiotic regimens for postpartum endometritis.Cochrane Database of Systematic Reviews2015, Issue 2. Art. No.: CD001067. DOI: 10.1002/14651858.CD001067.pub3.Link to Cochrane Library. [PubMed]
- https://www.researchgate.net/publication/7652898_Postpartum_Hemorrhage_After_Cesarean_Delivery_An_Analysis_of_Risk_Factors [accessed Jun 24 2018].
- Lynch J,Scholz S. [Anaesthetic-related complications of caesarean section]. [Article in German]. Zentralbl Gynakol.2005 Apr;127(2):91-5.
The Human Papillomavirus & The Cervical Cancer Connection
Rebecca B. Singson, M.D., F.P.O.G.S
Cervical cancer is the most common cancer in the female reproductive system. It is the second most common cancer afflicting females second only to breast cancer. What most people don’t realize is that cervical cancer is now recognized to be the first identified virally induced cancer in women. Research over the last few years has provided overwhelming evidence that infections with a high risk type of cancer-inducing Human papillomavirus (HPV) is necessary for the development of cancer. Understanding what can cause it and knowing how to monitor cervical cancer progression makes it one of the most highly preventable cancers afflicting the female.
Was the Pap Smear Not Doing the Job?
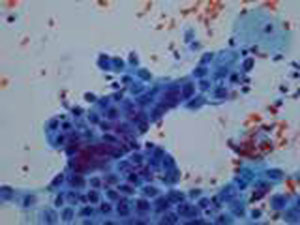
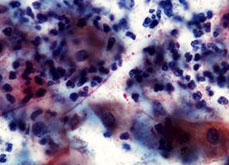
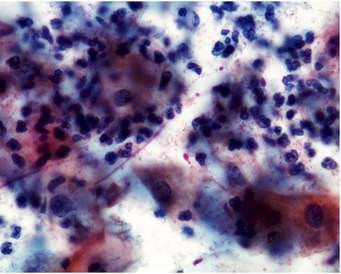
Fig 1. Pap smear under the microscope
There is no doubt that the introduction of cervical cytology introduced by Papanicolau (thus called the Pap smear), had a major impact in bringing about a significant reduction in the incidence of and mortality resulting from cervical cancer in many countries.3 Applying this massive screening program some fifty years ago has resulted in a 50-70% reduction of mortality resulting from cervical cancer. However, even in highly developed countries, this impact has not reached the desired levels expected from implementing a massive screening program because it has not resulted in the eradication of the disease and women are still dying from it.4
A recent critical review of evidence-based data showed that a single Pap smear misses up to 50% of cervical cancer precursor lesions.5 That’s one out of two!! Knowing this makes us now partly understand why cervical cancer continues to occur at such unacceptably high incidence rates, even in countries where the government spends money to subject its population to massive screening.
Understanding What Causes Cervical Cancer: the Viral Connection
Fig. 2. The humanpapillomavirus as seen on electron microscopy
Although the sensitivity of the Pap smear in picking up cervical cancer has not changed much in the last 10 years, there has been rapid growth in our knowledge as to what causes cervical cancer. Research has shown that the human papillomavirus is present in 99.7% of cervical cancers.2
What is this Wart-Causing Human Papillomavirus?
The human papillomavirus (HPV) is a double stranded DNA virus which infects the surface cells lining our tissues called epithelial cells. There are more than 70 distinct site-specific types (meaning they will grow on one part of the body but not on another). Of these, about 35 types are found in the anus and the genital areas, causing warts, also called condylomata acuminata and cervical cancer, the most notorious being types 16 and 18.

Fig. 3. Genital warts or condyloma acuminate caused by the HPV virus.
These infections are considered sexually transmitted and are among the most common sexually transmitted diseases in most countries affecting up to 40% of women with a yearly incidence of 10-15%6 . Many of the HPV infections do not show any signs of symptoms, and are therefore subclinical. It has been found that infections are relatively short-lived lasting usually 8-10 months.7 This indicates that our bodies are indeed capable of clearing the virus which is why in women over 30 years old, the prevalence drops down to 5-10%. Persistent infections, however, are found in 5-10% in women over 35 years old.6 It is in this group of women who are not able to clear the virus from their bodies that cancer in the cervix now has a chance to progress. Research in the last 10 years has consistently detected HPV in more than 90% of cases of cervical cancer, and in some studies, have found it in all cases.
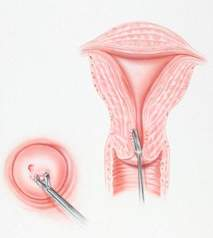
Is There a Way to Test if You are Positive for the Human Papillomavirus?
Because of advances in our knowledge linking the human papillomavirus to the causation of cervical cancer, it became necessary to develop HPV tests that would indicate if the woman was positive for the high-risk strains of the virus that would increase her risk for cervical cancer. The HPV DNA test is a commercially available test which tests for the presence of pieces of the HPV virus. It has has a sensitivity of >90%1 and a negative predictive value of over >90%.
The test entails taking cervical swabs, much like a Pap smear, using the brush from a cervical sampler. Pap smear collected with a broom collection device and rinsed in a solution in a plastic vial collecting system may also be used to provide the same specimen for HPV testing. Pap smears are still done in 2 ways: the conventional way is by smearing the cervical swab on a glass slide; the latest way is to use the broom collection device which immediately washed in a special fluid then run in a machine that filters out the cells from the solution and deposits them in a thin uniform monolayer of cells on a glass slide. The latter has the advantage of eliminating blood and musus from the specimen and makes it easier to examine under the microscope without the debris. The other advantage is that it can also provide the sample to test for HPV testing in case you deem it necessary. So, you can, in fact, ask your gynecologist to perform the test when you get your next Pap smear. Many recent studies have shown that the combination of HPV DNA test and Pap smear improves the detection rate of pre-cancerous lesions of the cervix compared to Pap smear alone.
What Does a Positive HPV Result Mean?
In women over 30, a positive result for high-risk types of HPVDNA means that she has a potentially persistent infection which means that she has a high risk of developing invasive cervical cancer. She should be immediately referred for colposcopy. This procedure involves looking at the cervix under high magnification, applying dyes to visualize abnormal cervical tissue and performing a biopsy, when necessary, of these abnormal areas. Women over 30 years old with a normal Pap smear but test positive for high-risk HPV have a 116-fold risk for developing high grade pre-cancerous lesions of the cervix compared to women who are HPV-negative.
Women in their 20s with a positive HPV DNA result should have a repeat HPV test after 9 months to one year. Since most HPV infections are transient, the virus should normally be cleared in 9 months, particularly in women younger than 30. If the test turns up to be negative, it means the infection has resolved and the woman can be monitored subsequently with Pap smears.
Are There Women Who Are At Increased Risk Than Others?
Since the virus is considered a sexually-transmitted disease, women who started having contact at an age earlier than 18 are at greater risk of acquiring the virus. Women who also have had more than 5 sexual partners or have had partners who have had more than 5 sexual partners are also at increased risk of being HPV positive.
It has been found that women who have had 5 vaginal births or more or have had a pregnancy before 18 yrs. are at increased risk of developing cervical cancer. It is possible that the immune state during pregnancy allows the virus to exert changes in the DNA of the cervical cells, thus, promoting cancer. It has also been found that smoking increases the risk of cervical cancer as well as having a partner who is not circumcised.
If any of the above conditions apply to you, it is best to test for HPV DNA in order to know your risk for developing precursor lesions in the cervix.
Our knowledge of cervical cancer has allowed man to create diagnostic tests that can determine a woman’s risk for developing cervical cancer. We are at an era where cervical cancer is a highly preventable disease. To die from it because we missed the test would be a crying shame.
Treatment
- LEEP – a loop electrosurgical excision procedure may be done to remove cervical lesions in the intra-epithelial stages before it becomes frank cancer. It is a conservative procedure especially for women desirous to preserve their fertility.
- Total hysterectomy – It is another form of management for cervical lesions before it becomes frank cancer. It involves the removal of the cervix and uterus. It may be done through an abdominal incision, transvaginally or minimally invasively using laparoscopic surgery or robotic surgery
- Radical hysterectomy, it is to remove cervix, uterus, upper vagina, ovaries, oviducts and affected lymph nodes. It may be done through open surgery with traditional abdominal incisions or with minimally invasive surgery using tiny, band-aid incisions using the Da Vinci (robotic surgery).
- Radiotherapy includes external radiation exposure and intra-cavitary irradiation. Cervical cancers from different stages can have radiotherapy. It may be a preferred option for patients with frank cancer who cannot tolerate surgery or whose cancer is beyond stage 2-A. It would, however, hurt the ovarian functions of females who undergo this before menopause.
- Chemotherapy for cervical cancer is the used of chemotherapeutic drugs for treatment, which is applicable to the patients from late stage or are suffering from recurrent cervical cancers. The side effects, however, are toxic and the patients may suffer more from that than the disease itself.
REFERENCES:
- National Institutes of Health (NIH) Consensus Development Statement1996.
- Walboomers JMMM, et al. Human papillomavirus, a necessary cause of invasive cervical cancer Worldwide. J Pathol.189:12-19 (1999).
- Hakama M, et al. Effect of organized screening on the risk of cervical cancer in the Nordic countries. In Miller AB, et al (eds.): Cancer Screening. Cambridge, Cambridge University Press, 1991: 153-162.
- Koss LG. The Papanicolau test for cervical cancerT detection: a triumph and a tragedy. JAMA1989; 261:737-43.
- Federal study shows conventional Pap test remains most effective was to diagnose cervical cancer. ACOG Today, March 1999, 43 (3).
- Shah KV, Howley PM Papillomavirus. In: Fields MN, et al, ed. Fields Virology, 3rd edition, Philadelphia: Lippencott Raven, 1988:2077-2109.
- Ho GYF, et al. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998; 338: 423-28.



















