THE DENTAL PREGNANT PATIENT
REBECCA B. SINGSON, M.D., FPOGS
Dental problems that may arise during pregnancy are given attention since it may also potentially affect the growing fetus. Here are some facts and problems for the dental pregnant patient to know
ARE DENTAL CARIES CONSIDERED AN INFECTIOUS DISEASE?
Dental caries is considered an infectious disease since it is caused by a bacteria called Streptococcus mutans which can be can potentially be transmitted to the fetus. If a pregnant mother has multiple caries in her mouth, it is not sufficient to do restorations or extractions since it won’t solve the problem. Unless she takes therapeutic measures during her pregnancy to diminish the bacterial load causing caries in her mouth, the baby is at risk of infection through the transplacental route. Vertical transmission of the mutans strep bacteria can occur from mother to child occurs after the eruption of the primary teeth.
WHAT ARE THE COMMON GUM DISEASES?
Normally, millions of microscopic monsters called bacteria make your mouth their home feeding on food particles left on our teeth. These bacteria produce acid as a result of their feasting and it is this acid which eats into tooth enamel creating cavities. If this wasn’t bad enough, the bacteria also pour out volatile sulfur compounds creating embarrassing bad breath. Normally bacteria are found within a mesh of mucus and debris known as plaque. Without regular dental hygiene these bacteria will multiply and pour out toxins causing gum inflammation leading to the following conditions:
- Pregnancy gingivitis can affect quite a number of pregnancies, some authorities saying at least half and other authorities saying even as much as a hundred percent of pregnant women. The changes in the gum are brought about by hormonal changes which alter the rate at which estrogen and progesterone are metabolized in the gums plus the change in prostaglandin synthesis. These affect the pregnant immune system altering the pattern and rate of collagen production in the gums which in turn, reduces the pregnant woman’s ability to repair and maintain gum tissue. Studies have shown that women with chronic gingivitis have an increased risk for preeclampsia, which is a pregnancy complication marked by swelling of the leg due to marked fluid retention, a rise in blood pressure and protein in the urine. The condition may lead to the more serious eclampsia where the pregnant woman goes in to convulsions compromising the fetus in the womb.
- Periodontitis – a chronic gingivitis may progress to a more serious condition if uncared for, where the infection can go beyond the bone and the tissues supporting it, leading to periodontitis. This can have serious implications on the pregnancy because research has shown that women with periodontitis are seven times more likely to have a premature delivery. Treating the condition can significantly decrease the risk because another research showed that pregnant women with preiodontitis who were treated with plaque & tartar removal called “scaling & planning” had significantly less preterm babies than women who were not treated.
SHOULD I TAKE FLOURIDE SUPPLEMENTS DURING PREGNANCY?
Most clinicians are not prescribing supplemental fluorides to pregnant women due to lack of evidence of efficacy for the unborn child. Also, it is important to note that current scientific evidence has demonstrated that prenatal fluoride supplements are not beneficial in preventing caries in the child’s primary dentition, and therefore are not prescribed to pregnant women. It was previously thought that fluoride could not pass through the placental barrier, but studies have shown that it does indeed cross the placental barrier. However, it is still not known how fast fluoride can transfer to the fetus by. Perhaps because fluoride gets diluted in the amniotic fluid, research shows that there is rapid maternal clearance with only a slight increase in fetal blood fluoride concentrations.
Since 1966, the Food and Drug Administration in the U.S.A. has banned the use of advertising and labeling of fluoride supplements for “prenatal use”. It has also banned claims that these supplements will prevent or reduce decay in the offspring of women who use them. The ban, however, does not prevent the prescription of fluoride supplements for pregnant women; it just restricts advertising claims until more solid evidence is available.
HOW CAN I CARE FOR MY TEETH DURING PREGNANCY?
- Brush your teeth at least twice daily. If you can brush after every meal and especially after indulging in sweets. An electric toothbrush cleans better than a manual toothbrush. Research shows that more dental plaque is dislodged with an electric toothbrush in 2 mins. than a manual toothbrush removed in 6 mins.
- Floss at least once a day as recommended by the American Dental Association. Flossing removes the bacteria that escape brushing by hiding in the tiny spaces between the teeth. Brushing without flossing is like washing only 65% of your body. The other 35% remains dirty!!
- Rinse with mouthwash or warm salt water. Warm salt water can help to soothe inflamed tissues.
- It is certainly best to visit your dentist regularly for professional teeth cleaning especially if you are contemplating a pregnancy. If you are already pregnant and have not ever seen a dentist, it is never too late. Make sure you tell your dentist you are pregnant and how many weeks of gestation so she may tailor your treatment without jeopardizing the baby.
You may not realize how important dental hygiene is to insure a non-complicated pregnancy. Healthy gums and healthy teeth in a pregnant mom is a vital component in having a healthy baby.
A DOCTOR’S POINT OF VIEW: CAN ABORTION HARM YOU?
Rebecca B. Singson, MD, FPOGS
In a Catholic country such as the Philippines where abortion is illegal, it is disgraceful to know that our abortion rates are even higher than in countries where abortion is freely and legally available. In the U.S.A, the reported abortion rate is 16 abortions/1000 women whereas in our country, the rate is a whopping is 20-30/1000 women. Some 400,000 abortions occur in our country every year. There is no question that backdoor abortions occur frequently such that 80,000 women per year are estimated to be treated in hospitals in the Philippines for complications of induced abortion.
HOW ITS DONE
Since the procedure is illegal in this country, you would think it would be very rare to find a doctor performing the procedure. However, a recent survey of health professionals in the Philippines suggests that about one-third of women seeking an abortion obtain it from a doctor or nurse which has reduced the proportion of complications requiring hospitalization in the last two decades. However, the majority of women still consult traditional practitioners or attempt through the use of prostaglandin medications to induce the abortion themselves. Based on the health professionals survey done in 1996, it is believed that untrained abortion practitioners in our country have increased their use of hormones and modern drugs aside from using traditional methods, such as abdominal massage.1 Usually midwives or hilots do the procedure in a house or sometimes clinic where they perform lower abdominal massage over the uterine area, prescribe some bitter herbs from quinine, or ask you to take some tablets orally or to insert some tablets vaginally to soften the cervix allow it to dilate. If that effects the bleeding, they may tell you to go to an obstetrician to complete the abortion or wait for spontaneous expulsion. If that does not work, the more dangerous procedure is to insert a rubber catheter (normally used for draining urine from the bladder) inside the uterus and keep it there for several hours to induce bleeding. It can be a painful experience since the foreign body in the uterus is intended to cause uterine contractions which feels like severe cramping or dysmenorrhea. Bleeding is always a desired result to effect expulsion of the products of conception.
THE DANGERS
Women who undergo abortion were found by research to be linked to certain behaviors such as smoking, drug abuse, eating disorders and promiscuity which all increase their risk for health problems. Teenagers comprise one-third of those who undergo abortion and are even at a much higher risk of suffering both immediate and long-term abortion-related complications.3 It was found that if the partner was present but not supportive, the miscarriage rate is more than double and the abortion rate is four times greater than if he was present and supportive. Absence or abandonment by the partner increases the abortion rate to 6 times greater.4
IMMEDIATE COMPLICATIONS:
Approximately 10% of women undergoing elective abortion will suffer immediate complications, of which approximately one-fifth (2%) are considered life threatening. The nine most common major complications which can occur at the time of an abortion are: infection, excessive bleeding, embolism, perforation of the uterus, anesthesia complications, convulsions, hemorrhage, injury to the cervix, and endotoxic shock. The most common “minor” complications include: infection, bleeding, fever, second degree burns, chronic abdominal pain, vomiting, gastro-intestinal disturbances.5
partner is present and not supportive, the miscarriage rate is more than double and the abortion rate is four times greater than if he is present and supportive. If the partner is absent the abortion rate is six times greater.” 5
HEMORRHAGE
Excessive bleeding due or after abortion may happen in the presence of cervical lacerations, uterine perforation, uterine atony or disorders in blood coagulation.
INFECTION
With the introduction of any foreign body into the uterus, the potential risk for infection increases. Post abortion, the patient may be at increased risk for infection of the uterus (endometritis), of the fallopian tubes (salpingitis) which may lead to ectopic pregnancies. Of patients who have a chlamydia infection at the time of the abortion, 23% will develop PID within 4 weeks. Studies have found that one-fourth to one-fifth of patients seeking abortion have a chlamydia infection and one-fourth of them will develop Pelvic Inflammatory Disease within 4 weeks. In the absence of Chlamydia, post-aborters will still develop PID.(11)
UTERINE PERFORATION
Between 2 and 3% of all abortion patients may suffer perforation of their uterus through the use of instruments,.The chances even increase
for those who were under general anesthesia during the abortion procedure or for those who had multiple deliveries.(5) (6) Damage to the uterus may eventually evolve into problems requiring a hysterectomy, if not reproductive or pregnancy problems.
CERVICAL DAMAGE:
During an abortion, the cervix may be forced open by an inexperienced practitioner causing cervical tears or permanent damage such as cervical incompetence leading to habitual abortion or premature delivery or labor complications.(7)
ECTOPIC PREGNANCY:
Abortion is significantly related to an increased risk of subsequent ectopic pregnancies. Ectopic pregnancies, in turn, are life threatening and may result in reduced fertility.(10)
CANCER RISK
Women with one abortion face a significant risk for cervical cancer, liver and ovarian cancer. One reason for this may be the due to the disruption of the hormonal changes which accompany a pregnancy..(4)
PLACENTA PREVIA:
Abortion increases the risk of placenta previa in later pregnancies. Abnormal development of the placenta due to uterine damage increases the risk of fetal malformation, perinatal death, and excessive bleeding during labor.(8)
Having an abortion can lead to many complications that can threaten the life of a woman and even ruin her chances of having a baby in the future. Remember that preventing a pregnancy can be much safer than trying to get rid of one.
- S. Singh, D. Wulf and H. Jones, “Induced Abortion in South Central and Southeast Asia: Results of a Survey of Health Professionals,” International Family Planning Perspectives, 23:59-67, 1997.
- Ibid.
- Wadhera, “Legal Abortion Among Teens, 1974-1978”, Canadian Medical Association Journal, 122:1386-1389,(June 1980).
- Ney, et.al., “The Effects of Pregnancy Loss on Women’s Health,” Soc. Sci. Med. 48(9):1193-1200, 1994; Badgley, Caron, & Powell, Report of the Committee on the Abortion Law, Supply and Services, Ottawa, 1997: 319-321.
- Frank, et.al., “Induced Abortion Operations and Their Early Sequelae”, Journal of the Royal College of General Practitioners (April 1985),35(73):175-180; Grimes and Cates, “Abortion: Methods and Complications”, Human Reproduction, 2nd ed., 796-813; M.A.
Freedman, “Comparison of complication rates in first trimester abortions performed by physician assistants and physicians,” Am. J. Public Health, 76(5):550- 554 (1986).
WHY SOME WOMEN DON’T BREASTFEED

Dr. Rebecca B. Singson, MD, FPOGS
- No pre natal preparation – many women get poor advise, or even no advise from their obstetrician during their prenatal check up. On the 1st meeting, ideally, the mother should already start psychological preparation for breastfeeding by reading books on breastfeeding, accessing websites on pregnancy & breastfeeding. It is never too early because those mothers who decide to breastfeed during the pregnancy are those who end up successfully breastfeeding. Especially with pregnancy adolescents, the chances of getting them to breastfeed increases over fourfold if they are given. Younger women and women with moderate to poor emotional support visitor were less likely to still be breastfeeding at three months.(Hodinott)
- No intrapartum/postpartum support – women who had a rough labor, prolonged labor and end up with a C-section usually want to sleep to recover from the exhausting experience and prefer to defer breastfeeding for a later time. Studies also show that mothers who spent 1 night in the hospital were almost twice as likely to breastfeed than mothers who spent 2 or 3 nights in the hospital. This may mean that hospitals, perhaps because of the Nursery set up, tend to separate the mother from the baby unless rooming- in occurs.(Margolis).
- Poor latch on – Women who experience pain when the baby starts to breastfeed and try to withstand the pain it instead or re-latching. can end up with cracked and sore nipples. This can result from wrong positioning of the baby. The mother & baby should ideally be in the tummy-to-tummy position with the ears of the baby directed to the ceiling. The baby’s mouth should include not only the nipple but the areola too and must not be allowed to tug on the nipple. Upon withdrawal of the nipple, it must not assume the shape of the end of a lipstick but should be a round structure.
- Wrong feeding pattern – Some women think that babies should feed only every two or 3 hours and only for 10-20 minutes. Babies should be fed on demand because it may take up to 2-4 weeks to establish a good milk supply. Most babies will gain weight if they are fed on demand or at least every 1 1/2 to 2 hours. Waiting more than 2 hours may cause the breasts to become engorged and painful. This decreases milk production. Women who think they will gradually build up breastfeeding by supplementing with formula or glucose water are setting themselves up for a higher likelihood of failure to establish breastfeeding. This is because introducing alternatives to breastmilk in the first 6 months will cause the baby to become full and decrease its demand of breastmilk which in turn will decrease its supply.
- ”Did not produce enough milk” – so many women are so insecure and so unempowered to believe that if nature had allowed them to bear a child, nature would also equip them with the means to keep their baby alive. It is all based on supply and demand. The moment you start to mix fix with formula, the demand for breastmilk decreases since the baby is fuller for a longer period of time. Logically, this is because the proteins of formula milk stay undigested for upto 60 mins (allowing the proteins to reach the intestines and cause major allergies) while breastmilk is digested within 15 mins.
- Unrelenting frustration – Women who end up with a comedy of errors that can start with a poor latch on then end up frustrated when she gets sore nipples or baby rejects her. The problem is the moment Mom gets stressed, she won’t release the hormone prolactin which is released from her pituitary gland at the base of the brain & is responsible for the milk let down reflex. .
- Poor home support – Some of the first people who may discourage you from breastfeeding may be your very own mother, aunt, or relative who grew up in a generation brainwashed by ads to believe that formula is superior to breastmilk. Some overbearing Moms may find it ridiculous why you should make like difficult for yourself when there is formula milk to free up your body and your time. This may lead one to believe that since your family members didn’t breastfeed you won’t be able to either (so untrue).
- Illness/infection – Sometimes a hospitalization for a serious illness, a fever or infection can prompt your pediatrician to shift you to formula feeding. Even during a fever or an infection, as long as it is not AIDS or active tuberculosis, one may continue to breastfeed. Research suggests strongly that any risk of transmission associated with breastmilk is negligible compared to the high risk of exposure to maternal blood and body fluids at birth. However, cracked or bleeding nipples or lesions with serous exudates could possibly expose the infant to infectious doses of Hep B.. (Stevens & Harvey)
- Work Interference – Many women stop breastfeeding once they go back to work 6-8 weeks after delivery. Leaking breasts can be embarrassing during a corporate meeting or the stress of the work itself can jeopardize the release of prolactin essential to the milk let-down reflex.
- Simply don’t want to – Some Women, however, who pregnant under adverse circumstances, like after a rape, are not psychologically prepared to breastfeed since they feel further violated..
- fear of pain – Those who imagine themselves being bitten on the nipples or have seen the suffering of some women with engorged nipples are afraid to undergo the experience themselves.
- uneasy with the thought – women don’t have the confidence that they have it within them to keep their baby alive through their natural faculty of breastfeeding.
- suits her lifestyle – some women don’t want to be tied down at home because of work or leisure reasons. Breastfeeding just simply cramps her style. The truth is, we can bring the baby everywhere and feed as needed. With a drape over your breast and the baby’s head, one can continue to breastfeed without even being noticed. All the baby really needs after all is is to be fed and changed.
- Our breastfeeding culture has disappeared – We live in a society where we do not see women breastfeeding if public. So if you haven’t grown up seeing women around you breastfeeding successfully, if it’s something that’s hidden away, then it becomes even harder for you to succeed yourself. Many women feel embarrassment with public exposure.
What Can Be Done?
- Consult a lactation consultant – a breast massage with lactation counseling does wonders to make your milk flow within the hour. Contact them through ReBirth Spa at 7719206/09178063339.
- Inquire about donated breast milk – If despite lactation counseling and best intentions, the milk is inadequate, (evidenced by less than 6-8 wet diapers per day after the 1st week, less than 3 stools in 24 hours or birth weight is not regained after the 10th day), you can ask your pediatrician or friends to patch you up with other breastfeeding moms willing to donate breast milk to you. It has been done and you can make it happen if you so desire.
Hoddinott P, Pill R, Hood K. Identifying which women will stop breastfeeding before three months in primary care: a pragmatic study. Br J Gen Pract 2000;50:888-91
Margolis LH, Schwartz JB. The relationship between the timing of maternal postpartum hospital discharge and breastfeeding. J Hum Lact 2000;16:121-8
Beasley PR, Shiao I-S, Stevens CE, Meng H-C . Evidence against breastfeeding as a mechanism for vertical transmission of Hepatitis B, , Lancet 1975;ii:740-41
Woo D, Davies PA, Harvey DR, Hurley R, Waterson AP . Vertical transmission of hepatitis B surface antigen in carrier mothers in two west London hospitals, , Arch Child Dis, 1979;54:670-75
HOW CAN YOU BE SO WRONG ABOUT BREASTFEEDING!

REBECCA B. SINGSON, M.D, FPOGS
In a third world country such as the Philippines where more than 50% of the population live below poverty line (defined in terms of a least-cost consumption basket of food that provides 2,016 calories and 50 grams of protein per day and of nonfood items consumed by families in the lowest quintile of the population) it is so disheartening, not to mention shocking to know that the minimum wage earner spends 26% of his wage buying formula milk when breast milk can guarantee less malnutrition, less diarrheal and upper respiratory infections for the neonate translating to less hospitalizations and best of all is available at no cost at all.
DID YOU KNOW?
Breastmilk is such a dynamic fluid that it is absurd to think that any brand of formula milk can even come close to it. The main proteins in milk are casein and whey (the more digestible between the two). The proportion of whey to casein differs in colostrum, in mature milk and in late lactation. The composition of breastmilk also varies during the time of the day and during the feeding. The hind milk (in the latter part of breastfeeding) has a much higher fat content than milk produced during the beginning portion of the feeding.(1) In fact, if your baby was premature, your breastmilk has a composition appropriate for premature babies. Furthermore, the odor and/or taste of breastmilk may change depending on the mother’s diet. Food preferences in adulthood are apparently developed in infancy so breastfeeding may actually help infants get used to different tastes and help prevent them from being picky eaters when they grow up.(2) How can any artificial milk formula duplicate these properties?
So dynamic and perfect is breastmilk as your baby’s food that you don’t need for any formula, glucose water, water, pacifier, teas, juices or vitamins during the first six months. Human milk has over 300 ingredients, including interferon, white blood cells, antibacterial and antiviral agents, while formula has only 40 ingredients. Breastmilk favors the growth of beneficial bacteria so breast-fed infants have a level of lactobacillus that is typically 10 times greater than that of formula-fed infants. This is the reason why they are better protected against diarrheal diseases. Because of the protective antibodies, your baby will have a much lower incidence of pneumonia and urinary tract infection if fed with breastmilk. In fact, adding formula milk in the first three months of life has been proven to triple the baby’s risk of getting admitted in the hospital for pneumonia (3). Furthermore, infants fed formulas of intact cow’s milk or soy protein compared with breast milk have a higher incidence of atopic dermatitis and wheezing illnesses in early childhood.(4)
BREASTFEEDING PROTECTS AGAINST CANCER
Did you know that breastmilk goes even so far as protecting the child from cancer before the age of 15? The risk of artificially fed children was 1-8 times that of long-term breastfed children. (5) And if that’s not reason enough for you, breastfeed for your own sake because breastfeeding confers some protection to you against uterine cancer (6), ovarian cancer(7) and breast cancer if you breastfeed for at least 2 years (but some benefit is already seen even if you only breastfed for 6 months). A study by Yale University researchers showed that women who breastfed for two years or longer reduced their risk of breast cancer by 50 percent (8).
LOCAL RESEARCH
In Baguio General Hospital & Medical Center (BGHMC), research shows that when they shifted over in 1975 from a practice of separating the mother and infant immediately after birth to a policy of immediate rooming in and breastfeeding, within two year time, breastfeeding increased from 40% to 92%. This simple practice also brought a dramatic reduction of mortality and morbidity because by 1977, the incidence of diarrhea droped from 27.5 to 1.5 per 1000 newborns and the mortality rate from diarrhea dropped from 8 per 1000 babies to none at all!(9)
KILLING THE INSTINCT TO BREASTFEED
Living in a civilized society has also killed our human instinct to breastfeed. Women are embarrassed to breastfeed in public and people are likewise uncomfortable to see a woman breastfeeding in public. Hospitals whisk out the baby to the nursery soon after birth separating the mother and baby. Although the Dept. of Health has implemented the Baby Friendly Initiative among hospitals to mandate rooming in immediately after birth, patients are made to sign waivers, oftentimes, without even explaining to them that the document they are signing is a consent NOT to room in the baby to actually allow milk formula to be given to their babies. In fact, soon after birth, the pediatrician is already discussing with the Mom what milk formula she would prefer to give the baby!! Family support is so hard to find since the now Mom’s own mother will discourage her from breastfeeding with words like “Bakit magpapakahirap ka pa eh may bote naman!” Many of our common practices with babies end up driving a wedge between Mommy and baby and keeps them separated. We create a separate Nursery room in the house for baby to stay in with her crib. We use a stroller to transport the baby instead of carrying her on a harness or sling like tribal societies do so the baby can sleep and breastfeed at will.
LACTATION SUPPORT
It is important that women feel supported during breastfeeding since many insecurities about her motherhood abilities surface when the going gets rough. Breastfeeding can cause a lot of distress to a Mom when her baby continues to cry despite giving her breast. Babies cry for many other reasons than hunger but Moms usually misinterpret this to mean, “I don’t have enough milk. My baby is starving.” The mere anxiety will interrupt the release of hormones that cause the letdown reflex of breastmilk thereby, decreasing the milk supply. In fact, research in Sweden has shown that every second mother experienced transient lactation crises on at least one occasion (the crisis group). The crises were mostly caused by emotional disturbances in the mothers (e.g. anxiety, stress and discomfort), or by the infant’s refusal to suckle, by unmotivated crying, or by illness. Within the crisis group no significant difference was found between the infants’ intake of breast milk during the crises compared with control measurements one week later. Nor had the crises any immediate impact on the growth of the infants. (10)
Research has shown that lactation counseling improves the rate of breastfeeding of women. (11)
The key to successful breastfeeding is the right preparation prior and during pregnancy, constant hydration and supplementation to sustain it, and when the going gets rough, seeking help from lactation therapists or other more experienced fellow breastfeeders.
- Lawrence RA and Lawrence RM. Breastfeeding, A Guide for the Medical Profession, 6th Ed. Elsevier Mosby, Phila, PA. 2005: p6-12, p73-86, p105-214, p377-388, p397-405, p747-749, p832-993
- Mennella JA and Beauchamp GK. Maternal diet alters the sensory qualities of human milk and the nursling’s behavior. Pediatrics. 1991: 88(4): 737-744.
- J.A. Cesar et al, Impact of Breastfeeding on Pneumonia on admission in the postnatal period in Brazil: Nested case control study, British Medical Journal, 1999 318:1316-20.
- Friedman NJ, Zeiger RS. The role of breast-feeding in the development of allergies and asthma..J Allergy Clin Immunol.2005 Jun;115(6):1238-48.
- Davis, M.K. Infant Feeding and Childhood Cancer. “Lancet 1988.
- Brock, K.E., “Sexual, Reproductive, and Contraceptive Risk Factors for Carcinoma-in-Situ of the Uterine Cervix in Sidney.”Medical Journal of Australia, 1989.
- Schneider, A.P. “Risk Factor for Ovarian Cancer. “New England Journal of Medicine, 1987.
- Tongzhang Zheng, et al., Lactation Reduces Breast Cancer Risk in Shandong Province, China. American Journal of Epidemiology Vol. 152, No. 12 : 1129-1135.
- Relucio-clavano N, How can hospitals encourage breastfeeding? Example from the Philippines. Mothers Child. 1982 Spring 2(2):4-5.
- Hillervik-Lindquist. Studies on perceived breast milk insuffienciency. A prospective study in a group of Swedish women.. Acta Paediatr Scand Suppl.1991;376:1-27.
- 11. Aidam BA, et al. Lactation counseling increases exclusive breast-feeding ratew sin Ghana. J Nutr. 2005 Jul;135(7):1691-5.
15 TIPS FOR CLUELESS DADS-TO BE

Dr. Rebecca B. Singson, M.D, FPOGS, FPSCPC
Many Dads get excited about the thought of having a baby yet are unaware of what it takes to support their wives during the pregnancy and postpartum process. Here are a few tips on how to maximize your role in the childbirth process:
- Suggest taking childbirth classes with your wife. It is a very empowering experience since it defines your role during the childbirth process.
- If you are unable to because of time constraints, just read up on books and the internet about the pregnancy and most especially, about the breastfeeding process so you can support your wife all the way through.
- Accompany your wife, whenever you can, to her pre-natal checkups.
- If you’re a first time Dad, practice carrying a baby using a doll so you won’t be too afraid to handle your own baby on the day of delivery. Ask your Mom, aunt, cousin or sister who is knowledgeable to teach you.
- Help your wife prepare her birth plan and, organize the things required on the day of labor, and what type of hospital room to choose.
- Moms experience a lot of discomfort and mood swings which may be hormonally related. Acknowledge her complaints and ask her what she would like you to do to help her. Most of the time, she just wants to be heard but is not looking for you to solve them. Be sympathetic at all times.
- Surprise her by sending her flowers or a nice basket of fruit (or a combination of both) on the day of her delivery with a love note telling her how much you appreciate her for fulfilling your life by bearing your child.
- Moms are so insecure about how they look during pregnancy, labor and after childbirth so keep reassuring her that she is just as beautiful and sexy in your eyes.
- Have a routine with your baby at a certain time like a feeding activity, or bathing with him daily or a regular playtime so you don’t feel left out.
- If you are still feeling left out, talk with your partner about it instead of harboring ill feelings and keeping it to yourself.
- Don’t be afraid to express your emotions. Talk to her doctor about your fears and concerns, if any. It’s also ok to cry as an expression of extreme joy at seeing your baby for the first time. For us women, it is not perceived as a sign of weakness but rather as a positive sign of sensitivity, which many men sorely lack.
- Support your wife throughout the breastfeeding process by encouraging her and letting her know how proud you are. Defend her from negative comments from well-meaning relatives about breastfeeding. Many relatives still carry the mistaken notion that cow’s milk is just as good or is even superior to mother’s milk.
- Your wife is in for years of many sleepless nights. Treat her to a pampering pre-natal or postpartum lactation massage. Rebirth Spa has therapists that can relax and support your wife through with her back pains and leg pains prior to giving birth as well as offer her lactation massage and counseling in the postpartum period. You may reach them through 7719204/06 or 0917-8063339. She will love you for it!
- If you have other kids, attend to them while Mom is attending to the baby. Your wife will appreciate your efforts in minimizing her distraction. Teach your kids that Mom needs to be in a relaxed state so the milk will flow to feed the baby. When Mom is tense, this can cut off the milk supply. That way you empower your kids to support Mom, too.
- Take out your wife to a romantic dinner without the kids at least once a month to help her regain her focus as wife and not just as a mother. She will appreciate the time away with you alone.
Having babies is a magical way of cementing your relationship and creating a stronger foundation of togetherness. Don’t let experience heighten your insecurity as a father or husband but rather use it as a platform to evolve to another level of maturity with your spouse. It can certainly do wonders in helping your relationship last a lifetime!
WATERBIRTHING: A NEW YET ANCIENT PHILOSOPHY ON CHILDBIRITH

REBECCA B. SINGSON, MD, FPOGS, FPSCPC

Waterbirthing is a non-traditional concept of giving birth which consists of the baby being delivered under water, careful monitoring and management of the process of labor, and restrictive use of invasive methods. The mother’s wishes are prioritized, the natural process of birth is respected, medical intervention and techniques are minimized as long as the safety of the mother and child are not compromised. The mother usually enters the birthing pool or tub during labor with the water set at body temperature once she goes in to active labor. She may go in and out as she pleases depending on the pace of her labor. She may opt to give birth in the water of out of it. She and her partner decide the process of her birth in conjunction with their doctor or birth attendant.
WHAT ARE THE ADVANTAGES OF WATERBIRTHING FOR LABORING WOMEN?:
Waterbirthing can provide the hydrothermal effects of producing perineal and vaginal relaxation. It also provides hydrokinetic effects of releasing oxytocin from the mother’s brain due to nipple stimulation of water. It minimizes the need for medical intervention because when the woman is relaxed, she experiences less pain, thus leading to less anxiety, which in turn lowers adrenaline levels, encouraging the release of oxytocin and more oxygen flow to tissues.
Compared to a laboring woman lying in bed with the uterus compressing the inferior vena cava (the biggest vein returning blood flow to the heart), water birthing lowers compression of the big vessels. Thus, blood supply to the uterus and the placenta is improved. This results in the fetus benefiting with improved oxygenation. 1
WHAT ARE THE ADVANTAGES FOR BIRTHING WOMEN AND BABY?:
Waterbirthing provides a low-risk alternative to delivering on bed or in a stirrup. The element of water angles the process of birth so it is viewed as a wellness rather than an illness. The process restores the control of the birthing process to the mother. Since the water duplicates the amniotic fluid environment inside the uterus, waterbirthing provides a gentle transition to the world for the baby instead of a violent one. It is said to foster non-violence in the child when he becomes an adult.2
A prospective study of more nearly 6,000 mothers giving birth was performed at the clinic for obstetrics & gynecology of the cantonal hospital of Fauenfeld, Switzerland comparing over 2000 waterbirths to other methods of delivery like the Maia-birthing stool, birthing bed, Roma wheel, and others. It was noted that waterbirthing was the most popularly chosen alternative birth method adopted by 34-40% of mothers with spontaneous single births. It was found that the episiotomy rates were lowest after waterbirths and the 3rd and 4th degree lacerations occurred less frequently than bedbirths.
There is also significantly lower blood loss in waterbirths which could be due to the lower incidience of perineal lacerations and the hydrostatic pressure in t the tub preventing vessels from bleeding.
Women who delivered by waterbirthing needed less painkillers compared to any other birth method. This had to do with the relaxing effects of water and the facilitated movement in its weightlessness.
The results in the neonates’ birth parameters such as pH of the arterial umbilical cord blood and Apgar scores were better than other birth methods. In over 2000 waterbirths in the study, there was not a single case of aspiration, drowning or death as a result of waterbirthing.
WHAT ARE THE CONTRAINDICATIONS TO WATERBIRTHING?
Waterbirthing is contraindicated in the presence of any documented fetal distress. Maternal fever of greater than 100.4 of suspected maternal infection or amnionitis or a positive HIV status also contraindicate waterbirthing. Vaginal, urinary tract and skin infections, excessive vaginal bleeding, heavy meconium staining or any conditions requiring continuous electronic fetal monitoring are also contraindications. Prematurity of the fetus and malpresentation also contraindicates waterbirthing. 1
WON’T MY BABY ASPIRATE OR DROWN DURING WATERBIRTHING?
There is no valid report of a neonate that ever drowned or died after birth as a consequence of a waterbirth.3 This has been explained by the diving reflex – and inhibitory reflex associated with the larynx. The larynx has been found to have 5x more taste buds than the whole tongue surface. When any liquid reaches the back of the throat, the taste buds interpret what substance it is and the glottis closes automatically so the liquid is swallowed, not inhaled. This reflex, which is present in all babies till age six to eight months to facilitate breastfeeding, prevents water aspiration.4
So under normal circumstances, the baby won’t breathe or gasp under water. It is only if the fetus was experiencing severe and prolonged lack of oxygen or because on anesthesia, that it may then gasp as soon as it is born, possibly inhaling water into the lungs.5
The baby continues to breathe while underwater through the placenta until the baby is brought out of the water. It is only when the face comes in contact with air that the first breath will be taken. One possibility why a baby would lack oxygen under water, though, would be if the placenta detached prematurely as in the case of abruptio placenta.
WON’T THE MOTHER OR BABY GET INFECTED?
Some hospital restrict a woman with a ruptured waterbag to do waterbirthing. There is really no basis for that since the research shows that the water does not enter the vaginal canal. In 1960, Dr. Siegel reported in the American Journal of OBGyn that when he did experiments on 30 moms to place tampons in the vaginal then have the mom sit in a tub of iodinated water for 15 mins., not one tampon became stained in all cases. He, thus, concludes that women should not be restricted from bathing in the later stages of labor.6
Infections of the neonate were not more frequent with a waterbirth delivery than any other birth method in over 2000 babies studied.3 There are some studies, though that show otherwise. 7.8
Studies show that women who give birth in water have the most satisfying birth experience.3 Waterbirthing is more a philosophy on nonintervention than a method of giving birth. It embodies spiritual, psychological, technological, humanitarian and scientific aspects of birth that make a mother completely connected to her body. It requires a certain level of consciousness and responsibility to take over her birth process and work with her doctor to avoid untoward outcomes that will jeopardize her baby. Waterbirthing is as ancient as it is new. Water allows us to surrender to the greatest miracle that can happen to a woman. The miracle of childbirth.

- Rossi A, Cornette J, Johnson MR, et al. Quantitative cardiovascular magnetic resonance in pregnant women: cross-sectional analysis of physiological parameters throughout pregnancy and the impact of the supine position. J Cardiovasc Magn Reson. 2011;13:31.
- 2 http://www.gentlebirth.org/archives/watrbrth.html. Birth Without Violence. Frederick Leboyer
- Geissbuhler Verena, Eberhard Jakob, Waterbirths: A Comparative Study. Fetal Diagn Ther 2000:15:291-300.
- Harding, R., Johnson, P., McClelland, M. (1978) Liquid sensitive laryngeal receptors in the developing sheep, cat and monkey. J of Physiol 277:409-22.
- Fewell, J.E. Johnson, P., Mc Clelland, M. (1983). Upper airway dynamics during breathing and during apnea in fetal lambs. J of Physiol 339:495-504.
- Siegel, P. (1960), Does Bath water enter the vagina? Journal of Obstet & Gynecol 15:660-1.
- Rawal J. Shah A, Stirk F, Mehtar S: Waterbirth and infection in babies, BMJ 1994;209-511
- Hawkins S: Water vs. conventional births; Infection rates compared. Nurs Times 1995-91:38-40.
Labiaplasty
Labiaplasty is a plastic surgery procedure which involves altering the labia minora (inner labia) and the labia majora(outer labia), the folds of skin surrounding the vulva.
Labiaplasty has been practiced since the 1970’s when women thought that the labia minora should not protrude beyond the labia majora for aesthetic and fuctional satisfaction.1
Because there are not many images of the vulva on social media or even textbooks, women have limited access to knowledge on vulvar anatomy. Therefore, they are unable to say what a “normal” vulva looks like. Because pornographic images are so easily available on the internet, this is likely the probable source of comparison of women of their vulvar structures and it is not uncommon for a woman, dissatisfied with her anatomy to bring a photo from a porn site to demonstrate how they would like their genitals to look like.
In 2005, a study was reported on measurements of the average size, color and texture of the various parts of the female vulva and the following table was published at the British Journal of Obstetrics & Gynecology2:
Measurements |
Mean [standard deviation] | |
| Clitoral length (mm) | 5.0 – 35.0 | 19.1 [8.7] |
| Clitoral glans width (mm) | 3.0 – 10.0 | 5.5 [1.7] |
| Clitoris to urethra (mm) | 16.0 – 45.0 | 28.5 [7.1] |
| Labia majora length (cm) | 7.0 – 12.0 | 9.3 [1.3] |
| Labia minora length (mm) | 20 – 100 | 60.6 [17.2] |
| Labia minora width (mm) | 7.0 – 50.0 | 21.8 [9.4] |
| Perineum length (mm) | 15.0 – 55.0 | 31.3 [8.5] |
| Vaginal length (cm) | 6.5 – 12.5 | 9.6 [1.5] |
| Tanner Stage (n) | IV | 4.0 |
| Tanner Stage (n) | V | 46 |
| Color of the genital area
compared to the surrounding skin (n) |
Same color | 9.0 |
| Color of the genital area
compared to the surrounding skin (n) |
Darker color | 41 |
| Rugosity of the labia (n) | Smooth (unwrinkled) | 14 |
| Rugosity of the labia (n) | Moderately wrinkled | 34 |
| Rugosity of the labia (n) | Markedly wrinkled | 2.0 |
Despite this, there is still no current established aesthetic ideal as to how the labia minor should look like. However, it is a common consensus that labia minor protruding past the labia majora are both aesthetically and functionally considered unsatisfactory. Aside from the labia minora, the labia majora has also been perused especially when porn centerfold photography started to show the female genitalia more prominently than the female breast.
Because of the huge variations in the vulvar anatomy, a patient’s expectations have to be managed and tailored towards realistic expectations because just like with plastic surgery of the face, one cannot convert an Oprah Winfrey to an Angelina Jolie.
TECHNIQUES FOR LABIAPLASTY:
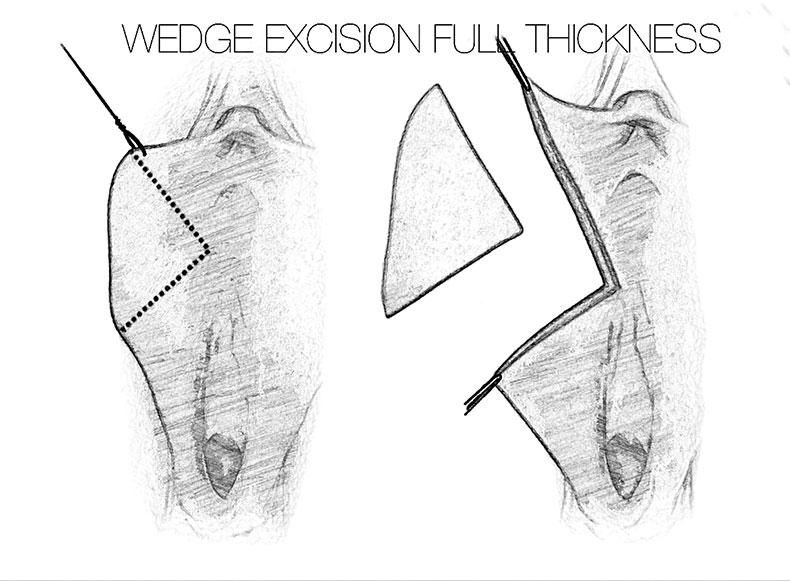
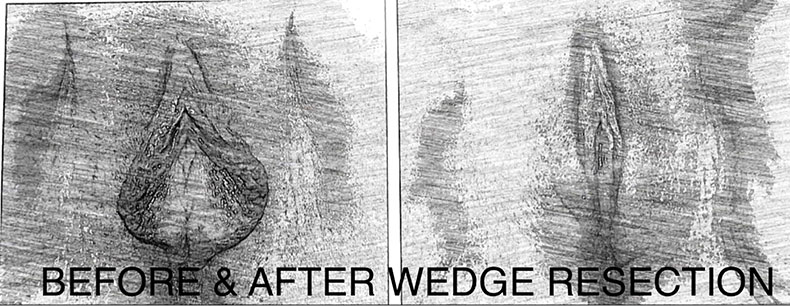
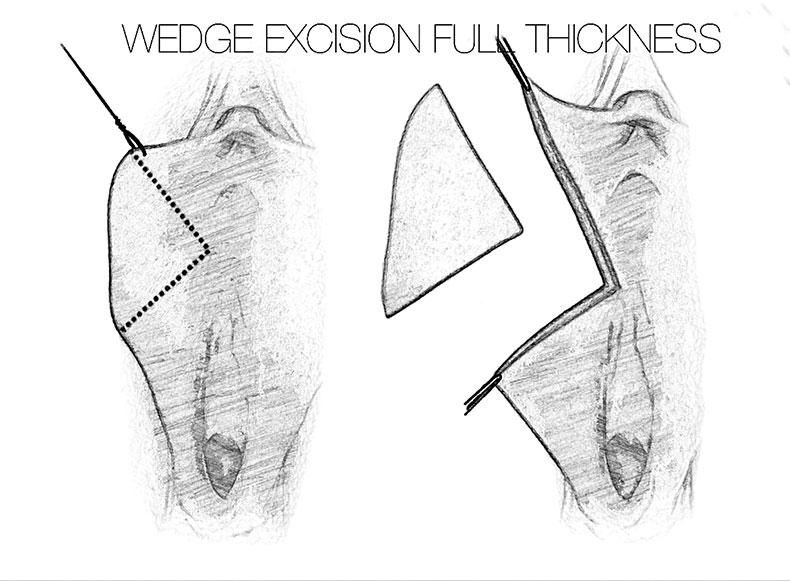
Wedge resection technique
It is rare for women who want labiaplasty to want to preserve the pigmented edge of their labia. For these cases, a wedge resection is ideal because central wedge-resection involves cutting and removing a partial-thickness wedge of tissue from the thickest portion of the labium minus. Unlike the edge-resection technique, the resection pattern of the central wedge technique preserves the natural rugosity (“wrinkled” edge) of the labia minora. If performed as a full-thickness resection, there is the risk of damaging some labial nerves, which can result in painful neuromas and numbness. A partial thickness removal of mucosa and skin, leaving the submucosa intact, decreases the risk of this complication.3 Furthermore, the central wedge-resection technique can be a tricky procedure since it is sometimes difficult to estimate the correct amount of labial skin to remove, so there is always the risk of either under-correction (persistent tissue-redundancy), or the overcorrection (excessive tension to the surgical wound),which may lead to increased probability either dissatisfaction or surgical wound dehiscence. One benefit, though is that extended wedge can be brought upwards towards the prepuce to treat a prominent clitoral hood without needing to create a separate incision.4 This leads to a natural contour for the finished result, and avoids direct incisions near the highly-sensitive clitoris.
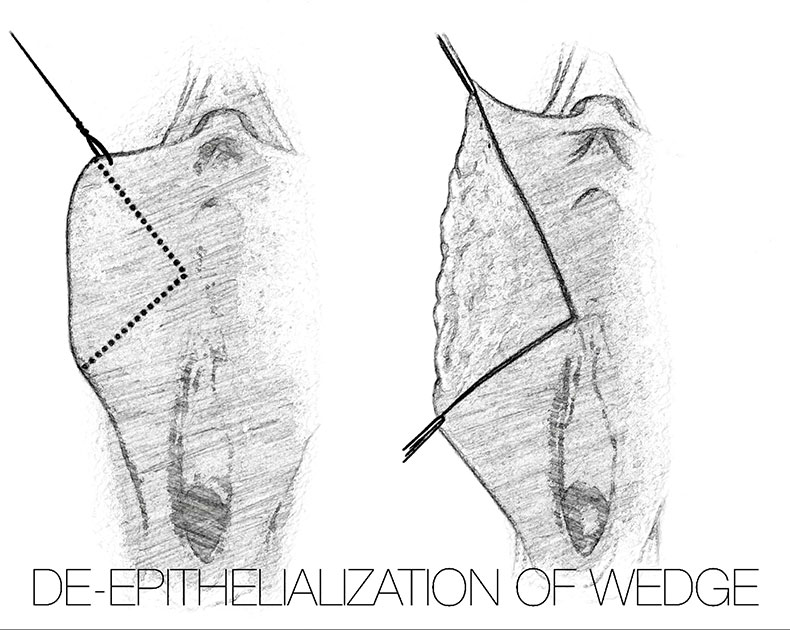
De-epithelialization/Demucosalization technique
For women with thin or atrophic labia, labial reduction by means of the de-epithelialization of the tissues is ideal. It involves cutting the epithelium of a central area on the inside and outside part of each labium minora, either with a scalpel or, low current pinpoint cautery, radiofrequency or laser knife. This method reduces the vertical excess tissue, while preserving the natural rugae (corrugated free-edge) of the labia minora. It plumps up the tissues since only the outer skin is removed plus it preserves the sensory and erectile characteristics of the labia. The disadvantage, though, of de-epithelialization is that the width of the individual labium might increase if a large area of labial tissue must be de-epithelialized to achieve the labial reduction.
Labiaplasty with Clitoral Unhooding
 Patients with large labia minora may also have a redundant or widened clitoral hood. This is where a labial reduction procedure may include the resection of the clitoral prepuce or clitoral hood when the thickness of its skin is considered unaesthetic to the patient or partner, or if it interferes with the woman’s sexual response. 5,6
Patients with large labia minora may also have a redundant or widened clitoral hood. This is where a labial reduction procedure may include the resection of the clitoral prepuce or clitoral hood when the thickness of its skin is considered unaesthetic to the patient or partner, or if it interferes with the woman’s sexual response. 5,6
Many waxing salons are sprouting in many countries, which Increases the awareness of women to wax their pubic hair. More women are choosing to use tight fitting gym outfits, swimwear and garments which can lead to more complaints of the labia minora getting caught mechanically or being abraded. It is also natural that women are getting more conscious of how their genitals appear.
Proper counseling needs to be given to women to assess the severity or deviation from normal anatomy, potential complications discussed before subjecting women to any procedure.
- Hamori CA. Aesthetic surgery of the female genitalia:labiaplasty and beyond. Plast Reconstr Surg 134:661, 2014.
- Lloyd, Jillian; Crouch, Naomi S.; Minto, Catherine L.; Liao, Lih-Mei; Creighton, Sarah M. (May 2005). “Female genital appearance: “normality” unfolds”. BJOG: An International Journal of Obstetrics & Gynaecology. Wiley. 112(5): 643–646.doi:10.1111/j.1471-0528.2004.00517.x. PMID15842291. Pdf.
- Alter, Gary J. (March 1998). “A new technique for aesthetic labia minora reduction”. Annals of Plastic Surgery. Wolters Kluwer. 40(3): 287–290.doi:10.1097/00000637-199803000-00016. PMID9523614.
- Alter, Gary J. (December 2008). “Aesthetic labia minora and clitoral hood reduction using extended central wedge resection”. Plastic and Reconstructive Surgery. Lippincott Williams & Wilkins. 122(6): 1780–1789.doi:10.1097/PRS.0b013e31818a9b25. PMID19050531.
- Hamori, Christine A. (1 September 2013). “Postoperative clitoral hood deformity after labiaplasty”. Aesthetic Surgery Journal. Oxford Journals. 33(7): 1030–1036.doi:10.1177/1090820X13502202. PMID24005612
- Hunter, John G. (1 September 2013). “Commentary on: postoperative clitoral hood deformity after labiaplasty”. Aesthetic Surgery Journal. Oxford Journals. 33(7): 1037–1038. doi:10.1177/1090820X13503476. PMID24081697.
10 SEXUAL TRUTHS YOU MUST KNOW

REBECCA B. SINGSON, MD, FPOGS, FACS, FPSCPC
- Men need to be wound up and excited during sex for them to achieve orgasm while women need to be relaxed with their partners to enjoy sex and reach peak pleasure.
- A man’s pleasure in sex is in the release of tension. He can go from foreplay to orgasm within 2 minutes. In contrast, a woman’s pleasure is in the gradual build-up of sexual tension and in fact, generally needs at least 20 mins. of foreplay before being ready for actual intercourse. She is like an oven than needs pre-heating. This is where a lot of men fall short. They think when they’re ready, their partner is ready. Unless the woman is dripping with lubrication, don’t attempt at intercourse because it’s a sign that her body in not ready. Doing so prematurely can lead to pain and laceration.
- There is an important purpose for this prolonged foreplay for women. There are 4 phases of the Human Sexual Response: the Excitement Phase, the Plateau Phase, the Orgasmic Phase and Resolution Phase. Excitement Phase is the phase of seduction which leads to the congestion of the organs. It takes around 20 mins. to get from Excitement Phase to Plateau Phase at which time the lower part of the vagina engorges to create friction (resulting in increased pleasure for the man), as well as for the vagina to lengthen. Vaginal lengthening is essential prior to intercourse because if the man starts thrusting before his partner’s vaginal canal has lengthened, he can induce a laceration at the end of the vagina and cause massive bleeding which has resulted at times in an emergency situation requiring suturing. (In my practice of 20 years, I have seen and managed 4 cases).
- Effective foreplay begins in the brain before you even touch each other’s bodies. Sexual turn ons for the woman: giving flowers, holding her hand, hugging her, complimenting her and her looks with big words like, “You are extremely irresistible”, “Your lips are so luscious”, “I’ve never met a sexier woman”. For the man, it’s rubbing his ego, allowing him his space, complimenting him on how good he is at turning you on. A sure turn off for a lot of men would be to choreograph his moves and be judgmental of him.
- Generally, a man’s satisfaction in sex relies in his ability to please his woman. A woman’s satisfaction in sex is in how well a man pleasures her. Or course, there are variants and extremes depending on how selfish or egoistic a person is.
- Orgasm for women is the release of sexual tension involving a response of all the muscles surrounding the vagina, anus and the uterus, contracting and repeating at 0.8 second intervals. The actual number and intensity of contractions varies from one woman to another but the important thing to remember is that the intensity of orgasm depends on the length of the Excitement Phase. That’s why it’s so important to spend a lot of time in foreplay because the longer and more excited you get your female partner to be, the more intense and pleasurable her orgasm will be.
- Orgasm is controlled by the sympathetic portion of the nervous system. This means that if you take some drugs like antihypertensives , or a big dose of alcohol which affect the sympathetic portion of the nervous system, it may interfere with your ability to achieve orgasm.
It had long been known that the center for orgasm of women was the clitoris until Grafenberg described the G-spot, which can be located this way: with the woman lying on her back, if her partner inserts a finger in the vagina with the palm facing the ceiling, on the anterior wall of the vagina within an inch from the opening, you can feel a 1×1 cm rough ridge, which when stimulated gives the woman the sensation she wants to pee. When stimulated rapidly alternating with or without clitoral stimulation, it can lead to an intense orgasm. - At the height of orgasm, some women release ejaculatory fluid from the urethra akin to the male prostatic fluid. It can be a generous amount and so may lead the woman and her partner to think she may have urinated. But in the absence of the smell of urine, this has got to be ejaculatory fluid.
- After an orgasm, women generally have no refractory period before reaching their next orgasm. Thus women can be multi-orgasmic. The men, in contrast, have a refractory period and need a period of time before achieving their next orgasm.
- Sexual satisfaction is one of the most important human experiences. However, as much as 50% of all married couples experience some sexual dissatisfaction, yet rate themselves to be happily married. This implies that sexual satisfaction not a necessary component to a happy marriage.
For women in menopause, hormone replacement therapy may greatly enhance a woman’s libido, promote vagina lubrication and prevent the vaginal atrophy that happens with the drop of estrogen. The thinning out of the vaginal walls results in dyspareunia or painful intercourse. This can be reversed with estrogen replacement which may be given Italy, transdermally or transvaginally.
Aside from hormones, vagina lasers administered intravaginally once a month for three months of the year can also promote vaginal lubrication and thickening, enhancing sexual satisfaction, removing the pain with intercourses, tightening the vagina after childbirth, and reversing mild to moderate incontinence (involuntary passing of urine when you cough or sneeze after childbirth.
Management of Uterine Fibroids
For over 100 years, surgery was the mainstay of treatment of uterine fibroids or myomas. Up until recently, therapeutic management of symptomatic uterine fibroids was broadened to three pillars: surgery, pharmacotherapy, and interventional radiotherapy. Nearly 50% of hysterectomies done for benign reasons are due to myomas.1
American data reveals that myomas occur in about 60% of African-American women and in upto 40% or Caucasian women aged 35. The incidence goes even higher at age 50 to around >80% in Black women and 70% of Caucasian women. Sex hormones have been implicated to cause the growth of myomas.2 Thus, when a woman is approaching menopause which is at an average of 49 or 50 among Filipinos, the drop in hormones may actually save her from hysterectomy depending on the size of the myoma and severity of symptoms such as bleeding and pain.
SIGNS & SYMPTOMS. Signs and symptoms of myomas vary. More than size, location of the myomas in the uterus vary since very large myomas up to 16-20 cm located at the outermost layer of the uterus called the serosa, have gone unnoticed, especially if the patient is obese. Conversely, even a 1 cm. myoma can cause vaginal bleeding if located in the cavity of the uterus. The patient may also experience pelvic pain if the myoma causes pressure on the nearby organs. If a bulky tumor grows forward and applies pressure on the urinary bladder in front it, the patient may experience frequency of urination, or inability to completely empty the bladder or inability to sleep due to constant bathroom trips. If the bulky tumor presses on the back of the uterus, it can impinge on the intestines and cause constipation. Myomas may also cause infertility and frequent miscarriage. Myomas or polyps are found in nearly 30% of women with recurrent miscarriage. 3,4
DIAGNOSIS. The gold standard for diagnosis is still the transvaginal ultrasound for non-virgins, or transrectal ultrasound in virgins. However, if the uterus rises above the pelvis and may be too large for the vaginal probe to reach, a pelvic or transabdominal ultrasound is done. A Magnetic Resonance may also help visualize the position, relations to the adjacent structures and actual number.
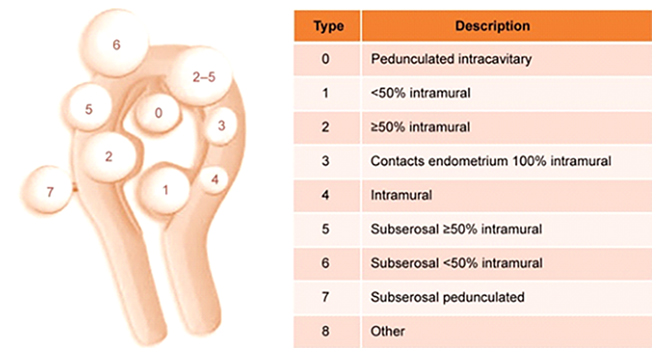
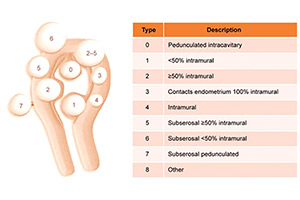
Figure 1
The International Federation of Gynecology and Obstetrics classification system for uterine fibroids.5
FIGO classification of uterine fibroids according to Munro et al. (2011). Fibroid types range from 0 to 8. 0 = Pedunculated, intracavitary; 1 = Submucosal, <50% intramural; 2 = Submucosal, ≥50% intramural; 3 = Contact with endometrium, 100% intramural; 4 = Intramural; 5 = Subserosal, ≥50% intramural; 6 = Subserosal, <50% intramural; 7 = Subserosal, pedunculated; 8 = Other (e.g. cervical, parasitic). Where two numbers are given (e.g. 2–5), the first number refers to the relationship with the endometrium, while the second number refers to the relationship with the serosa; e.g. 2–5 = Submucosal and subserosal, each with less than half the diameter in the endometrial and peritoneal cavities respectively. Fibroid classification cartoon republished with permission from Munro et al. (2011).
CONSERVATIVE MANAGEMENT
Patients who present with bleeding were usually offered tranexamic acid for 3-4 days monthly. It is a drug that promotes coagulation that has has been proven to reduce blood loss during menstruation. It is very well tolerated with few side effects.6,7.
The levonorgestrel intrauterine (LNG-IUS) has also been used successfully in bleeding patients with myomata.8 However, the presence of a submucous myoma distorting the uterine cavity may prevent a gynecologist from actually inserting the device properly.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are also commonly used especially for patients with pain/and or bleeding in addition to hormones, either estroprogestins or progestogens, acting on the endometrium. Although it does not directly affect the fibroid to shrink it, it can reduce menstrual blood loss in women with mild and even severe bleeding. It is well tolerated as long as taken with food.9
Until 2012, GnRH agonists were the only therapeutic drugs approved for the treatment of myoma. The use of GnRH analogues reduces fibroid size and
bleeding symptoms. They act by reducing estrogen concentrations in the blood serum to postmenopausal levels. The side effects may be undesirable since it causes menopausal symptoms like hot flushes, skin and vaginal dryness, mood swings, loss of libido, vaginosis, depression, and bone loss. GnRH agonists are usually administered as subcutaneous injections for 3-4 months prior to surgery and they are not recommended for long-term use.
However, GNRH agonists have been losing ground because of their side effects such as hot flushes and bone loss plus the advent of a newer, cheaper drug that can be taken orally instead of subcutaneous injection. 10The new drug is ulipristal acetate (UPA), a selective progesterone receptor modulator oral drug, which can cause the bleeding from myomas to stop after 7 days of use and up to a 51% reduction in fibroid size after 13 weeks of use. By giving UPA tablets prior to Laparoscopic or Robotic surgery of large masses, shrinkage of the mass may actually happen with less possibility for anemia and blood transfusion since the bleeding pre-operatively may also be stopped. Another advantage of this drug versus the GNRH agonists is that the blood levels of estrogen remain higher similar to the estrogen levels women have in the first half of the menstrual cycle. This therefore means that there are less side effects such as thromboembolism and osteoporosis which are inherent to GNRH agonists. Side effects with multiple treatments of UPA are usually headaches, nasal congestion and sore throat, abdominal pain, and hot flushes. Because a greater number of
progesterone receptors have been found in myomata compared to normal uterine tissue another advantage of UPA is that it induces cell death or “apoptosis”. Therefore, unlike GNRH agonists, where the myoma shrinks only while you are taking the drug then grows back again to the previous size when you stop the drug, with UPA, the fibroid shrinkage persists for 6 mos. after stopping the drug. UPA, however, causes thickening of the lining of the uterus. Therefore, the drug is administered for three months then rest for two months before resuming the drug for three months again. 12
However, following recent reports of 4 women who developed severe liver failure while on UPA, 3 ending up with a liver transplant, on February 2018 the Medicines & Healthcare products Regulatory Agency (MHRA) advised of new temporary safety measures for ulipristal acetate13 following reports of serious liver injury in women using the medicine for uterine fibroid
The temporary safety measures are:
- Not to initiate new prescriptions for ulipristal acetate even for women who have already one or two courses of the drug previously.
- Monitor all women on the drug with liver function tests at least once a month. Stop UPA treatment in any woman who develops transaminase levels more than 2 times the upper limit of normal, closely monitor and refer for specialist hepatology evaluation as clinically indicated. Repeat liver function tests in all women 2 to 4 weeks after stopping treatment.
- For any recent or present users of UPA with signs or symptoms suggestive of liver injury (such as nausea, vomiting, malaise, right hypochondrial pain, anorexia, asthenia, jaundice), check transaminase levels immediately, If transaminase levels are more than 2 times the upper limit of normal, stop treatment, closely monitor and refer for specialist hepatology evaluation as clinically indicated.
- Advise women using UPA on the signs and symptoms of liver injury.
UTERINE ARTERY EMBOLIZATION
Uterine artery Embolization is a procedure where small polyvinyl particles are delivered via a catheter to the uterine arteries inserted on the femoral artery by an interventional radiologist. By doing so, the blood supply to the uterine fibroid is blocked, resulting in shrinkage, not disappearance of the myoma. It is indicated in women who have a major contraindication to undergo a surgery, or in women who strongly want to keep their uterus. Although it is considered a fertility-sparing procedure, it is, not recommended if a woman is desirous of pregnancy since she may actually drop her ovarian reserve.
Some of the side effects may include pain which results from occluding the blood supply, fever, infection and sepsis. The data also shows that if one resorts to a uterine fibroid embolization, the chances are higher that a patient may require a further surgery in two years which compared to women who underwent a straight myomectomy or an outright hysterectomy.14
HIGH INTENSITY FOCUSED ULTRASOUND (HIFU)
In contrast to Uterine Artery Embolization, HIFU uses no radiation. Rather, it acts much like the principle of using the magnifying glass to focus sunlight and burn paper. Focused ultrasound makes use of an acoustic lens to concentrate multiple intersecting beams of ultrasound on a target. Each single beam can pass through tissues with little effect but at the focal point where the beams all converge, the energy can generate heat high enough to ablate fibroids and cause cell death, blast ovarian cysts and even get rid of kidney stones.
On Oct. 2004, the US FDA first approved the HIFU for treatment of symptomatic uterine fibroids. The HIFU has been shown to be a safe and effective morality in achieving symptomatic relief while avoiding the risks inherent to surgery or other invasive therapies.15 Upto 16-20% will require additional intervention. 13
SURGICAL TREATMENT HYSTEROSCOPY
Hysteroscopic enucleation of a myoma is possible if the location of the myoma is inside the uterine cavity, the submucosal type. The patient usually comes to the clinic with complaints of bleeding. In fact, 59.8% of patients with myoma who present with vaginal bleeding actually have a submucosal myoma.16 It may also be discovered in patients who cannot get pregnant and in those with recurrent spontaneous abortion.17,18 Patients who have submucosal uterine fibroids may be attributed to dysregulated uterine contractility.19
In 20% of infertile patients, intrauterine fibroids or polyps are diagnosed.17,20 After hysteroscopic resection of intrauterine myoma, pregnancy rates
reach about 50%21 and bleeding symptoms are resolved in 70-99% of cases.18
As previously presented, we go back to the International Federation of Gynecology & Obstetrics classification of myoma:
• Type 0: the myoma is located completely in the uterine cavity or pedunculated.
• Type 1: <50% of the myoma is located in the myometrium.
• Type 2: >50% of the myoma is located in the myometrium.
It is important to determine this in order to predict the possibility for complete resection of the myoma prior to the procedure. According to European Society of Hysteroscopy (ESH) in 2012, this is the percentage success rate for complete resection of a myoma:
• Type 0: 96-97%
• Type 1: 86-90%
• Type 2: 61-83%
The success of surgery & rate of complete resection correlates inversely with the size of the myoma.22 An infertile patient diagnosed with a submucous myoma, even if it is less than 1.5 cm in size and without symptoms, must be subjected to a hysteroscopic myomectomy because the chances of success in pregnancy are high. In dealing with Type 2 myomas larger than 4 cm in size, a higher level surgeon expertise and experience is required since the complication rate increases with longer operating time. Since fluid is constantly infused into the uterine cavity in the course of the hysteroscopic myomectomy, there is a risk for fluid overload that can be fatal if unmonitored. 23