Recurrent Pregnancy Loss
One of the most distressful phenomena that can happen to a couple trying to conceive is a recurrent pregnancy loss (RPL), which can happen to 2-5% of couples. A miscarriage or spontaneous abortion, is defined as the loss of a clinical pregnancy before 20 completed weeks of gestational age (18 weeks after fertilization) or, if gestational age is unknown, the loss of an embryo/fetus of <400 g.1
Pregnancy loss is actually more common than we think since only 30% of all conceptions result in a live birth.2 Many pregnancies fail before we even detect a positive pregnancy test. Many women think they just had delayed menses but actually, it was an undetected miscarriage. Among the pregnancies we recognize clinically approximately 15% of them result in spontaneous abortion, there are many more pregnancies that fail prior to being clinically recognized.
Nearly half of these are unexplained and the other half are due to causes such as, antiphospholipid syndrome, hormonal and metabolic disorders, uterine anomalies and cytogenetic abnormalities. Other etiologies have been proposed but are still considered controversial, such as chronic endometritis, inherited thrombophilias, luteal phase deficiency, and high sperm DNA fragmentation levels.
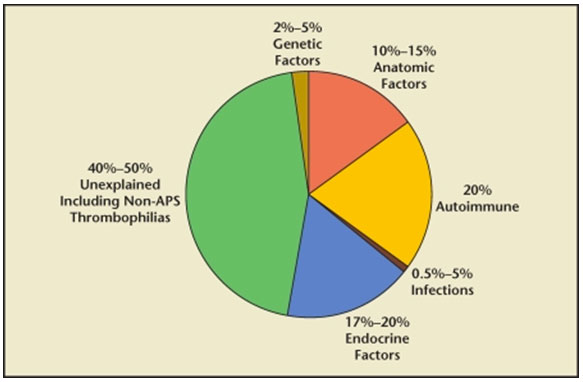
FIG 1. Causes of Infertility.3
ANATOMIC CAUSES
Uterine anomalies are reportedly found in up to 19% of women with RPL and can be classified as acquired or congenital.4
Uterine anomalies are thought to cause miscarriage by interrupting the blood supply of the endometrium, resulting in abnormal placental development. Among the congenital anomalies, the presence a septum in the cavity of the uterus is the one of the most notorious in causing as much as a 76% risk of spontaneous pregnancy loss among affected patients.5 Other uterine anomalies, like the unicornuate, didelphic, and bicornuate uteri have been found to cause less risk for recurrent pregnancy loss.6 Asherman’s Syndrome, or intrauterine adhesions/scarring or synechiae, is an acquired uterine condition, when the front and the back walls of the uterine cavity stick to the each other resulting from overcurettage in evacuating a pregnancy after a miscarriage or after an infection in the lining of the uterus, called endometritis. This may also result in recurrent pregnancy loss. Myoma, a benign tumor in the muscle of the uterus, also called fibroids, if located inside the cavity of the uterus or if located in the muscle of the uterus and are larger than 5 cm, can also cause recurrent pregnancy loss by competing for the blood supply needed for implantation.7
HORMONAL/ENDOCRINOLOGIC CAUSES
Among the endocrinologic disorders implicated in recurrent pregnancy loss, approximately 17% to 20% are found to be due to luteal phase defect (LPD), polycystic ovarian syndrome (PCOS), diabetes mellitus, thyroid disease, and hyperprolactinemia. 8,9
Polycystic Ovary Syndrome has been found in at least 40% of women with RPL 10 , as well as poorly controlled type 1 diabetes.11 The fact that patients improve and miscarry less when on an insulin sensitizing drug, metformin, leads to the theory that insulin resistance and the resultant hyperinsulinemia that is often present in cases of PCOS and type II diabetes mellitus might be a mechanism responsible for causing recurrent pregnancy loss in these patients.12
Hypothyroidism has been associated with spontaneous abortion and RPL.13 but even patients with normal thyroid levels but with antithyroid antibodies have been found to become hypothyroid soon after they get pregnant.14 Pregnancy outcomes in these women may improve with early (possibly prenatal) thyroid hormone replacement.15 The most commonly used criteria to define subclinical hypothyroidism is a serum thyroid-stimulating hormone (TSH) threshold of >2.5 mIU/L. 16
Uncontrolled diabetes has been shown to increase the risk of miscarriage, whereas maintaining good control of sugar before attempting to get pregnant significantly shinks the risk back to normal.17,18
Progesterone deficiency or Luteal Phase Defects, because of its effect on the endometrium in the second half of the menstrual cycle after ovulation happens, called the luteal phase, can impair normal implantation. Many mechanisms, such as inadequate follicular growth, dysfunctional ovulation, poor corpus luteum function, and abnormal endometrial response and receptivity, have been proposed.19,20
Elevated prolactin hormone levels have been found to cause infertility and RPL. altering the hormonal balance and feedback mechanisms involving the hypothalamic–pituitary–ovarian axis, which can lead to impaired formation of eggs in the ovary and failure to ovulate.21
IMMUNOLOGIC CAUSES
As human beings, we are equipped with an immunologic system that protects us from getting ill when invaded by foreign proteins, viruses and bacteria. If you think about it, the fetus is actually a foreign protein with a different genetic material from the mother. How is it then that a pregnancy woman is able to tolerate a foreign protein to grow inside her? That’s because there are many mechanisms and alterations in our immune system to allow us to carry a foreign protein with a different genetic make-up inside our bodies. When some of these mechanisms fail, it also results in failure to implant or to carry the baby to term. One specific auto-immune disorder leading to recurrent pregnancy loss is the Anti-phosopholipid antibody syndrome (APS). It is prevalent in 3% to 5% in the general population and is characterized by the presence of at least 1 clinical and 1 laboratory criterion.22
Diagnostic criteria for APS according to “the International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome”:
| At least 1 clinical and 1 laboratory criteria must be present for definite APS |
|
|---|---|
| Clinical criteria |
|
| I – Vascular thrombosis |
One or more clinical episodes of an arterial, venous, or small vessel thrombosis, in any tissue or organ. Thrombosis must be confirmed by imaging or Doppler studies or |
| histopathology, with the exception of superficial venous thrombosis. For histopathologic confirmation, thrombosis should be without significant evidence of inflammation in the vessel wall. |
|
| II – Obstetric morbidity |
1) One or more unexplained demise of a morphologically normal fetus at or beyond 10 weeks of gestation, with normal fetal morphology documented by ultrasound or by direct examination, or 2) One or more premature births of a morphologically normal neonate before the 34th week of gestation, because of a) eclampsia or severe preeclampsia or b) placental insufficiency, or 3) Three or more unexplained consecutive miscarriages of <10 weeks of gestation. Known factors associated with recurrent miscarriage, including parental genetic, anatomic, and endocrinologic factors should be ruled out. |
| Laboratory criteria |
I – aCL (IgG and/or IgM) in the blood, present in medium or high titers (> 40 GPL or MPL or >99th percentile), on two or more occasions, at least 12 weeks apart, measured by a standardized ELISA. II – Anti-β2GP1 antibody of IgG and/or IgM isotype in the blood (>99th percentile) on two or more occasions, at least 12 weeks apart, measured by a standardized ELISA. III – Lupus anticoagulant present in plasma, on two or more occasions at least 12 weeks apart, detected according to the guidelines of the International Society on Thrombosis and Hemostasis. |
Abbreviations: APS, antiphospholipid syndrome; aCL, anticardiolipin antibody; ELISA, enzyme-linked immunosorbent assay.
LIFESTYLE FACTORS
Several lifestyle factors have been associated with an increased risk of miscarriage: Obesity, defined as a body mass index >30 kg/m2,23,24 smoking,25 excessive caffeine consumption (>300 mg/day, or the equivalent of two cups), excessive alcohol intake,25,26 and cocaine.27 Patients with recurrent pregnancy loss should be advised to modify their lifestyle to avoid these factors.
Genetic factors
The vast majority of early pregnancy losses (50%–60%) are the consequence of chromosomal abnormalities, which can be inherited from either parental, or arise spontaneously in the embryo from parents with normal chromosomes.28.29
Because of the principle of survival of the fittest and natural selection, up to 90% of embryos which contain any abnormal chromosomes are spontaneously aborted. The most commonly found abnormalities are numeric chromosome errors, such as trisomy, polyploidy, and monosomy X. The risk of aneuploidy significantly increases with maternal age.17,28,30,
DIAGNOSIS AND TREATMENT:
It is not recommended to evaluate a couple following one miscarriage.31
it is acceptable to start a workup following two consecutive losses, especially in women aged >35 years.17,31
A thorough gynecologic history should be obtained, as well as a family history of infertility or miscarriage. Both partners should also be questioned about the modifiable lifestyle factors, such a smoking, alcohol use, and nutritional habits as well as presence of genetic problems in the family.17,31,32,33
Diagnostic evaluation for uterine anatomic anomalies should include office hysteroscopy or hysterosalpingography (HSG). Hysteroscopic resection of intrauterine adhesions and intrauterine septa are indicated if these abnormalities are identified. Patients undergoing successful hysteroscopic septum resection seem to enjoy near normal pregnancy outcomes, with term delivery rates of approximately 75% and live birth rates approximating 85%.34 Myomectomy should be considered in cases of submucosal fibroids or any type fibroids larger than 5 cm. Resection has been shown to significantly improve live birth rates from 57% to 93%.35 Depending on the size and location, myomectomy can be performed via the following modalities: robotic surgery, laparoscopy, open laparotomy, or hysteroscopy.
For APAS patients with RPL, tests for anticardiolipin antibodies and lupus anticoagulant should be included. Treatment should include low-dose aspirin (LDA, 81–100 mg/d) plus prophylactic low-molecular-weight heparin in otherwise healthy women without a history of of a systemic autoimmune disease such as systemic lupus erythematosus, or a history of thrombosis. Low dose aspirin
should be started before conception or with a positive pregnancy test. Heparin treatment should be started with a positive pregnancy test.36 Heparin is a large complex of molecules that do not cross the placenta and, as such, is regarded as safe during pregnancy.
For endocrine evaluation, prolactin levels can be tested three hours from waking up, thyroid hormones without any preparation. For women with elevated prolactin levels, called hyperprolactinemia and RPL, treatment with drugs like bromocriptine 2.5–5 mg/day until 9th week of gestation, significantly decreased miscarriage rates compared to no treatment.37
For cases of Polycystic ovary, the diagnosis is clinched with the presence of two out of three criteria: 1. irregular menses, 2. evidence of high levels of testosterone like hirsutism, acne or elevated testosterone hormone level; 3. Polycystic ovaries by ultrasound. Therapy involves weight management, when overweight or obese, and giving with insulin sensitizing drugs like metformin, and progesterone treatment. Other relevant tests may be a Thyroid-stimulating Hormone evaluation, Anti-Mullerian hormone evaluation to check for ovarian reserve, serum prolactin in patients with irregular menses, anti-thyroid antibody testing and endometrial biopsy when indicated, to evaluation luteal phase defects.
For luteal phase defects, Progesterone supplementation is the most widely used treatment because of its availability, ease of administration, and tolerability.
UNEXPLAINED RECURRENT PREGNANCY LOSS
Despite all the work-up, almost half of patients will remain without a definitive diagnosis and unexplained causes. It remains unclear how to best manage these patients although Progesterone treatment has been found to be of benefit in decreasing the miscarriage rate among women who have experienced at least 3 losses.38 Low-dose aspirin has also been investigated as a potential therapy for unexplained RPL. Its use prior to and during pregnancy has only been proven to increase live birth rates among those women with previous miscarriages beyond 13 weeks of gestation.39,40
ON A POSITIVE NOTE
Despite the depression that couples feel after recurrent pregnancy losses, it might help to focus on the fact that there is still a high probability of success on a subsequent pregnancy. it can be helpful for the physician and patient to keep in mind the relatively high likelihood that the next pregnancy will be successful. Overall, the prognosis for RPL is encouraging. Even with the diagnosis of RPL and as many as 4 to 5 prior losses, a patient has a greater than 60% to 65% chance of carrying her next pregnancy to term.41
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. International Committee for Monitoring Assisted Reproductive Technology; World Health Organization. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524. [PubMed]
- Macklon NS, Geraedts JPM, Fauser BCJM. Conception to ongoing pregnancy: the “black box” of early pregnancy loss. Hum Reprod Update. 2002;8:333–343. [PubMed]
- Ford HB, Shust DJ. Recurrent Pregnancy loss: Etiology, Diagnosis & Therapy. Rev Obstet Gynecol. 2009 Spring; 2(2): 76–83.
- Jaslow CR, Carney JL, Kutteh WH. Diagnostic factors identified in 1020 women with two versus three or more recurrent pregnancy losses. Fertil Steril. 2010;93(4):1234–1243. [PubMed]
- Raga F, Bauset C, Remohi J, et al. Reproductive impact of congenital Müllerian anomalies. Hum Reprod. 1997;12:2277–2281. [PubMed]
- Lin PC. Reproductive outcomes in women with uterine anomalies. J Womens Health. 2004;13:33–39.[PubMed]
- Bajekal N, Li TC. Fibroids, infertility and pregnancy wastage. Hum Reprod Update. 2000;6:614–620.[PubMed]
- Stephenson MD. Frequency of factors associated with habitual abortion in 197 couples. Fertil Steril.1996;66:24–29. [PubMed]
- Fox-Lee L, Schust DJ. Recurrent pregnancy loss. In: Berek JS, editor. Berek and Novak’s Gynecology.Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 1277–1322.
- Rai R, Backos M, Rushworth F, Regan L. Polycystic ovaries and recurrent miscarriage—a reappraisal.Hum Reprod. 2000;15:612–615. [PubMed]
- Mills JL, Simpson JL, Driscoll SG, et al. Incidence of spontaneous abortion among normal women and insulin-dependent diabetic women whose pregnancies were identified within 21 days of conception. N Engl J Med. 1988;319:1617–1623. [PubMed]
- Glueck CJ, Wang P, Goldenberg N, Sieve-Smith L. Pregnancy outcomes among women with polycystic ovary syndrome treated with metformin. Hum Reprod. 2002;17:2858–2864. [PubMed]
- Vaquero E, Lazzarin N, De Carolis H, et al. Mild thyroid abnormalities and recurrent spontaneous abortion: diagnostic and therapeutical approach. Am J Reprod Immunol. 2000;43:204–208. [PubMed]
- Poppe K, Velkeniers B, Glinoer D. The role of thyroid autoimmunity in fertility and pregnancy. Nat Clin Pract Endocrinol Metab. 2008;4:394–405. [PubMed]
- Negro R, Formoso G, Coppola L, et al. Euthyroid women with autoimmune disease undergoing assisted reproduction technologies: the role of autoimmune disease and thyroid function. J Endocrinol Invest. 2007;30:3–8. [PubMed]
- De Groot L, Abalovich M, Alexander EK, et al. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab.2012;97(8):2543–2565. [PubMed]
- Practice Committee of the American Society for Reproductive Medicine Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98(5):1103–1111. [PubMed]
- Jovanovic L, Knopp H, Kim H, et al. Elevated pregnancy losses at high and low extremes of maternal glucose in early normal and diabetic pregnancies: evidence for a protective adaptation in diabetes. Diabetes Care. 2005;28(5):1113–1117. [PubMed]
- Jones GS. The luteal phase defect. Fertil Steril. 1976;27(4):351–356. [PubMed]
- Li TC, Spuijbroek MD, Tuckerman E, et al. Endocrinological and endometrial factors in recurrent miscarriage. BJOG. 2000;107(12):1471–1479. [PubMed]
- Bussen S, Sütterlin M, Steck T. Endocrine abnormalities during the follicular phase in women with recurrent spontaneous abortion. Hum Reprod. 1999;14(1):18–20. [PubMed]
- Derksen RHWM. The obstetric antiphospholipid syndrome. J Reprod Immunol. 2008;77:41–50.[PubMed]





