The Human Papillomavirus & The Cervical Cancer Connection
Rebecca B. Singson, M.D., F.P.O.G.S
Cervical cancer is the most common cancer in the female reproductive system. It is the second most common cancer afflicting females second only to breast cancer. What most people don’t realize is that cervical cancer is now recognized to be the first identified virally induced cancer in women. Research over the last few years has provided overwhelming evidence that infections with a high risk type of cancer-inducing Human papillomavirus (HPV) is necessary for the development of cancer. Understanding what can cause it and knowing how to monitor cervical cancer progression makes it one of the most highly preventable cancers afflicting the female.
Was the Pap Smear Not Doing the Job?
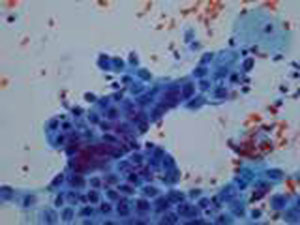
Fig 1. Pap smear under the microscope
There is no doubt that the introduction of cervical cytology introduced by Papanicolau (thus called the Pap smear), had a major impact in bringing about a significant reduction in the incidence of and mortality resulting from cervical cancer in many countries.3 Applying this massive screening program some fifty years ago has resulted in a 50-70% reduction of mortality resulting from cervical cancer. However, even in highly developed countries, this impact has not reached the desired levels expected from implementing a massive screening program because it has not resulted in the eradication of the disease and women are still dying from it.4
A recent critical review of evidence-based data showed that a single Pap smear misses up to 50% of cervical cancer precursor lesions.5 That’s one out of two!! Knowing this makes us now partly understand why cervical cancer continues to occur at such unacceptably high incidence rates, even in countries where the government spends money to subject its population to massive screening.
Understanding What Causes Cervical Cancer: the Viral Connection
Fig. 2. The humanpapillomavirus as seen on electron microscopy
Although the sensitivity of the Pap smear in picking up cervical cancer has not changed much in the last 10 years, there has been rapid growth in our knowledge as to what causes cervical cancer. Research has shown that the human papillomavirus is present in 99.7% of cervical cancers.2
What is this Wart-Causing Human Papillomavirus?
The human papillomavirus (HPV) is a double stranded DNA virus which infects the surface cells lining our tissues called epithelial cells. There are more than 70 distinct site-specific types (meaning they will grow on one part of the body but not on another). Of these, about 35 types are found in the anus and the genital areas, causing warts, also called condylomata acuminata and cervical cancer, the most notorious being types 16 and 18.

Fig. 3. Genital warts or condyloma acuminate caused by the HPV virus.
These infections are considered sexually transmitted and are among the most common sexually transmitted diseases in most countries affecting up to 40% of women with a yearly incidence of 10-15%6 . Many of the HPV infections do not show any signs of symptoms, and are therefore subclinical. It has been found that infections are relatively short-lived lasting usually 8-10 months.7 This indicates that our bodies are indeed capable of clearing the virus which is why in women over 30 years old, the prevalence drops down to 5-10%. Persistent infections, however, are found in 5-10% in women over 35 years old.6 It is in this group of women who are not able to clear the virus from their bodies that cancer in the cervix now has a chance to progress. Research in the last 10 years has consistently detected HPV in more than 90% of cases of cervical cancer, and in some studies, have found it in all cases.
Is There a Way to Test if You are Positive for the Human Papillomavirus?
Because of advances in our knowledge linking the human papillomavirus to the causation of cervical cancer, it became necessary to develop HPV tests that would indicate if the woman was positive for the high-risk strains of the virus that would increase her risk for cervical cancer. The HPV DNA test is a commercially available test which tests for the presence of pieces of the HPV virus. It has has a sensitivity of >90%1 and a negative predictive value of over >90%.
The test entails taking cervical swabs, much like a Pap smear, using the brush from a cervical sampler. Pap smear collected with a broom collection device and rinsed in a solution in a plastic vial collecting system may also be used to provide the same specimen for HPV testing. Pap smears are still done in 2 ways: the conventional way is by smearing the cervical swab on a glass slide; the latest way is to use the broom collection device which immediately washed in a special fluid then run in a machine that filters out the cells from the solution and deposits them in a thin uniform monolayer of cells on a glass slide. The latter has the advantage of eliminating blood and musus from the specimen and makes it easier to examine under the microscope without the debris. The other advantage is that it can also provide the sample to test for HPV testing in case you deem it necessary. So, you can, in fact, ask your gynecologist to perform the test when you get your next Pap smear. Many recent studies have shown that the combination of HPV DNA test and Pap smear improves the detection rate of pre-cancerous lesions of the cervix compared to Pap smear alone.
What Does a Positive HPV Result Mean?
In women over 30, a positive result for high-risk types of HPVDNA means that she has a potentially persistent infection which means that she has a high risk of developing invasive cervical cancer. She should be immediately referred for colposcopy. This procedure involves looking at the cervix under high magnification, applying dyes to visualize abnormal cervical tissue and performing a biopsy, when necessary, of these abnormal areas. Women over 30 years old with a normal Pap smear but test positive for high-risk HPV have a 116-fold risk for developing high grade pre-cancerous lesions of the cervix compared to women who are HPV-negative.
Women in their 20s with a positive HPV DNA result should have a repeat HPV test after 9 months to one year. Since most HPV infections are transient, the virus should normally be cleared in 9 months, particularly in women younger than 30. If the test turns up to be negative, it means the infection has resolved and the woman can be monitored subsequently with Pap smears.
Are There Women Who Are At Increased Risk Than Others?
Since the virus is considered a sexually-transmitted disease, women who started having contact at an age earlier than 18 are at greater risk of acquiring the virus. Women who also have had more than 5 sexual partners or have had partners who have had more than 5 sexual partners are also at increased risk of being HPV positive.
It has been found that women who have had 5 vaginal births or more or have had a pregnancy before 18 yrs. are at increased risk of developing cervical cancer. It is possible that the immune state during pregnancy allows the virus to exert changes in the DNA of the cervical cells, thus, promoting cancer. It has also been found that smoking increases the risk of cervical cancer as well as having a partner who is not circumcised.
If any of the above conditions apply to you, it is best to test for HPV DNA in order to know your risk for developing precursor lesions in the cervix.
Our knowledge of cervical cancer has allowed man to create diagnostic tests that can determine a woman’s risk for developing cervical cancer. We are at an era where cervical cancer is a highly preventable disease. To die from it because we missed the test would be a crying shame.
Treatment
- LEEP – a loop electrosurgical excision procedure may be done to remove cervical lesions in the intra-epithelial stages before it becomes frank cancer. It is a conservative procedure especially for women desirous to preserve their fertility.
- Total hysterectomy – It is another form of management for cervical lesions before it becomes frank cancer. It involves the removal of the cervix and uterus. It may be done through an abdominal incision, transvaginally or minimally invasively using laparoscopic surgery or robotic surgery
- Radical hysterectomy, it is to remove cervix, uterus, upper vagina, ovaries, oviducts and affected lymph nodes. It may be done through open surgery with traditional abdominal incisions or with minimally invasive surgery using tiny, band-aid incisions using the Da Vinci (robotic surgery).
- Radiotherapy includes external radiation exposure and intra-cavitary irradiation. Cervical cancers from different stages can have radiotherapy. It may be a preferred option for patients with frank cancer who cannot tolerate surgery or whose cancer is beyond stage 2-A. It would, however, hurt the ovarian functions of females who undergo this before menopause.
- Chemotherapy for cervical cancer is the used of chemotherapeutic drugs for treatment, which is applicable to the patients from late stage or are suffering from recurrent cervical cancers. The side effects, however, are toxic and the patients may suffer more from that than the disease itself.
REFERENCES:
- National Institutes of Health (NIH) Consensus Development Statement1996.
- Walboomers JMMM, et al. Human papillomavirus, a necessary cause of invasive cervical cancer Worldwide. J Pathol.189:12-19 (1999).
- Hakama M, et al. Effect of organized screening on the risk of cervical cancer in the Nordic countries. In Miller AB, et al (eds.): Cancer Screening. Cambridge, Cambridge University Press, 1991: 153-162.
- Koss LG. The Papanicolau test for cervical cancerT detection: a triumph and a tragedy. JAMA1989; 261:737-43.
- Federal study shows conventional Pap test remains most effective was to diagnose cervical cancer. ACOG Today, March 1999, 43 (3).
- Shah KV, Howley PM Papillomavirus. In: Fields MN, et al, ed. Fields Virology, 3rd edition, Philadelphia: Lippencott Raven, 1988:2077-2109.
- Ho GYF, et al. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998; 338: 423-28.





