Pap Smears: When and How Often?
Cervical cancer is the most common cancer in the female reproductive tract and is the second most common cancer in women next to breast cancer. It is however a more deadly cancer since for every 4 Filipinas who survive breast cancer, only 2 or 3 will survive cervical cancer. In Asia, there are 266,000 new cases of cervical cancer diagnosed each year. Of these, 7225 new cases are from the Philippines alone, according to our 2005 National Cancer Institute statistics. The sad thing is that two-thirds of these cases are diagnosed at a late stage when they are beyond the operative stage such that 32.3% of them die in 1 year and 73% will die in 5 years.
In developed countries where medicine is socialized and where mass screening with Pap smears is mandated, the incidence of invasive cervical cancer has declined tremendously. This is because the disease is caught at a pre-cancerous or early stage where the disease can still be eradicated without major surgery.
WHAT IS THE PAP SMEAR?
The conventional Pap smear is most inexpensive screening test for cervical cancer. It involves taking a sample of cells from the cervix (which is the opening of the uterus) either with a brush, a spatula or a cotton swab, smearing this on a glass slide and fixing it with a solution so the Pathologist can look under the microscope for any cancerous cells or signs of infection. Conventional pap smear, however have a high failure rate, and is estimated from 50-80% accurate. A new method of Pap smear called the liquid based pap test has improved accuracy by about 54%.
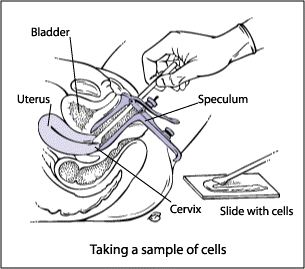
Fig 1. How to perform a Pap smear.
With the liquid-based pap test, the cells taken from the cervix are rinsed in a small vial of special solution to preserve the cells. At the laboratory a machine is able to separate the blood and mucus from the cervical cells which are then tested for abnormalities. Research shows this new method of pap test significantly increases the ability of the doctor and laboratory to identify cervical abnormalities.
WHO SHOULD HAVE A PAP SMEAR AND HOW OFTEN?
In 2016 the American Cancer Society came out with the following guidelines for early detection of cervical cancer:
- All women should start having Pap smears from age 21-29 every three years. No HPV screening is necessary.
- From age 30-65, women are recommended to test for both the Pap smear and HPV test.. If the HPV test is negative, the Pap smear and HPV can be done every 5 years. However, for women who have certain risk factors such as diethylstilbestrol (DES) exposure before birth, HIV infection, or are immunocompromised due to, chemotherapy, chronic steroid use, or organ transplant should still continue to have annual Pap smears.
- Another option for women 30-65 years old is to have only Pap smear without HPV testing every three years
- For women over 30 years old with access to a center where the Human Papillomavirus is tested may opt for HPV testing. If found to be negative, they may be defer screening to every 5 years with either the conventional or liquid-based Pap test, plus the HPV DNA test.
- Women 65 years of age or older who have had regular screening for the last 10 years 3 or more normal Pap tests in a row and no abnormal Pap test results in the last 10 years may choose to stop having cervical cancer screening. Women with a history of cervical cancer, DES exposure before birth, HIV infection or a weakened immune system should continue to have screening as long as they are in good health.
- Women with a history of CIN2 or CIN3 should continue to have testing for at least 20 years after the abnormality was found.
- Women who have had a total hysterectomy (removal of the uterus and cervix) may also choose to stop having cervical cancer screening, unless the surgery was done for treatment for cervical cancer or for a precancerous lesion. Women who have had a hysterectomy without removal of the cervix should continue to follow the guidelines.
It is always helpful to tell women to see their gynecologist for an annual check-up on their birth month so they don’t ever forget that on their birthday, their gift to themselves is their health. Having a regular check up can help you catch cervical cancer before it catches you.
Indications, Risks and Benefits
Rebecca B. Singson, MD, FPOGS, FACS, FPSGE, FPSCPC
A Cesarean section or C section is a surgical delivery of one baby or multiple babies by cutting through the mother’s abdomen and the uterine wall. If the surgery is scheduled ahead of time, it is referred to as an elective cesarean section (as opposed to an unscheduled emergency Cesarean section). There has been an increased rate of Cesarean sections recently According to Williams Obstetrics, these are the following indications for C sections:
MATERNAL INDICATIONS
Prior Cesarean delivery – because of the scar in the uterus, there is a risk of uterine rupture if the mother goes into labor after a previous Cesarean delivery although it is said to be <1%.
Abnormal placentation – this may be due to placenta previa or placenta accreta. Placenta previarefers to low implantation of the placenta. It classically presents as painless vaginal bleeding in the third trimester secondary to an abnormal placentation near or covering the internal cervical os.
Placenta accreta is when the placentagrows too deeply into the uterine wall.It can cause massive bleeding usually after delivery, since the placenta fails to detach.
Maternal request – a mother may elect to deliver by C section before or after going into labor even when there is no firm indication for a C section. Women who desire elective primary Cesarean delivery should be presented with the advantages and disadvatages. Although a C section may offer decreased risks for hemorrhage and chorioamnionitis compared with a planned primary vaginal birth, it does carry with it the disadvantage of higher rates of maternal thromboembolism, hysterectomy, and re-hospitalization for infection or wound complications; longer initial hospital stays; and higher chances of uterine rupture or abnormal placental implantation in subsequent pregnancies.3,4,5 Women who undergo a Cesarean delivery are much more likely to be delivered by a repeat operation in subsequent pregnancies.
Another advantage of a Cesarean delivery is that it is associated with lower rates of urinary incontinence and pelvic organ or uterine prolapse.6,7,8,9,10
Prior classical hysterotomy the uterus – if there has been a previous Cesarean section where the uterus has been incised the Classical way, which means the uterus was incised in the contractile portion of the uterus, there is an indication to perform a subsequent Cesarean section. Because the risk of uterine rupture in women with prior Classical Cesarean deliveryis about 9%11 it may be prudent to schedule a repeat Cesarean deliveryat 36-37 weeks. The danger, though, is the higher risk for respiratory distress syndrome in the fetus.
Unknown uterine scar type – if a patient has undergone a previous surgery on the uterus whether for a removal of a myoma or a previous C section, or if it is unknown whether a low cervical Cesarean section or a Classical Cesarean section was performed, there is an indication to perform a repeat Cesarean section.
Uterine incision dehiscence – Cesarean section in advanced labor is associated with increased risk of incomplete healing of the uterine incision leading to uterine incision dehiscence. The reported incidence of this condition ranges between 0.2% and 4.3% of all pregnancies associated with a previous C section.12 A repeat C section is indicated to repair the thinned out uterine wall.
Prior full-thickness myomectomy – A myomectomy scars the uterus and increases the risk for uterine rupture with subsequent pregnancy if allowed to go into labor.
Genital tract obstructive mass – the presence of a myoma in the cervix, or a vaginal tumor would be some types of genital obstructive masses that would prevent a normal birth and would have to be delivered by C section.13
Invasive cervical cancer – Women with cervical cancer are better delivered by C section than by vaginal birth.The recommendation is based on the finding that women diagnosed with cervical cancer within 6 months after delivering a baby, particularly vaginally, had poorer survival and higher risk of recurrent disease than women who were diagnosed with cervical cancer during their pregnancy.
Prior trachelectomy – Patients who underwent removal of the cervix for benign or malignant reasons are better delivered by Cesarean section.
Permanent cerclage – patients with incompetent cervix with permanent cercalge to keep the cervix closed may undergo an elective C section.
Prior pelvic reconstructive surgery – there are some women, especially those with exposure to a drug called diethylstilbestrol, who develop abnormalities in their reproductive organs like a double uterus, or a uterus with a septum, etc. These can cause infertility and therefore, may need reconstruction to unify the uterus or remove the septum. In some procedures which involve cutting through the uterus to unify the two cavities, called the Strassman procedure, it will be necessary to deliver by Cesarean section to prevent the uterus from rupturing on or before labor.
Pelvic deformity – there are certain types of pelvic bones that cannot support a vaginal birth. In the past, this was validated by x-rays, called x-ray pelvimetry. But present practice guidelines no longer favor exposing the fetus to radiation but instead favoring a trial of labor and an eventual C section should labor not progress. The reason for this is that even if the x ray pelvimetry reports a contracted pelvis, but the fetus is small, the baby can still be successfully be delivered vaginally.
Herpes Simplex Virus infection – if active lesions are present at the onset of labor, a Cesarean section should be recommended to prevent the fetus from acquiring the virus.14 However, if the membranes have been ruptured for more than 6 hours, it is not certain that a Cesarean section would benefit the baby. A Cesarean section can reduce, but cannot totally eliminate, the risk of newborn infection.14,15. A recent study found that a Cesarean section delivery reduces the risk of HSV among newborns by 86%16.
Human Papilloma Virus infection – HPV DNA has been detected in amniotic fluid, placenta, and the umbilical cord.17 Both chorionic and placental tissue can be infected through the hematogenous (by blood) route and hence, HPV can be spread to amniotic cells that are then ingested by the fetus18,19. Another possible route of transmitting the HPV virus is through the placenta. The virus can possibly go up via the maternal genital tract, since it has been shown that the HPV-DNA can be present, both in amniotic fluid19 and the umbilical cord,18 in pregnant women with cervical intraepithelial lesions.
Cardiac disease – various researches bear out that women with heart disease end up with a Cesarean section more often then healthy women. 20,21 However, the fact is, in patients with cardiac problems, the preferred mode of delivery is via a vaginal birth, since a Cesarean section is associated with more blood loss and higher thromboembolic and infection risk. A Cesarean section in a woman with heart disease is reserved only for obstetric indications. Examples of situations in which primary a Cesarean section should be considered are: if a woman goes into labor while on oral anticoagulants (because of risk of fetal intracranial bleeding), Marfan syndrome with diameter of the ascending aorta >45mm, acute or chronic dissection, and acute heart failure.22
Pathology requiring concurrent intra-abdominal surgery – if a woman develops cervical or ovarian cancer that requires a hysterectomy after delivery of the baby, it is warranted to perform a CS hysterectomy.
Perimortem Cesarean delivery – In cases where the mother is dying or dies while pregnant from an accident, heart diseases or cancer, etc, the baby has to be evacuated as a life-saving measure.
MATERNAL-FETAL INDICATIONS
Cephalopelvic disproportion (CCPD)– it is a condition when a baby’s head or body is too big to fit through the mother’s pelvis. Many cases of “failure to progress” during labor are given a diagnosis of CPD. Risk factors for CPD are Estimated Fetal weight of > 3,000 g, pre-pregnancy body mass index (BMI) > or = 25 kg/m2, nulliparity (never been pregnant before) and the inadequacy of clinical pelvimetry.23
Failed operative vaginal delivery – In the past, the forceps and vacuum were used to deliver the head for the more difficult cases of cephalopelvic disproportion. As cesarean delivery became more widely available in the early to mid-20thcentury, new practices were developed to minimize morbidity and maximize safety of operative vaginal delivery.One such practice which evolved, is the concept of a trial of forceps or vacuum. This approach utilizes a double set- up such that if the forceps or vacuum fails, an immediate cesarean delivery can be done.24
Placenta previa or placental abruption – a low-lying placenta, especially if it covers part or all of the internal opening of the cervix necessitates delivery by Cesarean section. Abruptio placenta involves partial or total premature separation of the placenta while the fetus is still in the womb, thus, cutting the oxygen supply to the fetus. It is a dire, life-threatening emergency which may need immediate C section.
FETAL INDICATIONS
Non-reassuring fetal status – Late decelerations (drop in fetal heart rate below 120 beats/min), bradycardia (slowed heart rate) less than 70 beats per minute, and abnormal fetal heart rate patterns during the first stage of labor might jeopardize fetal well-being, and an expedited delivery should be considered.25
If a vaginal birth is not imminent and the forceps or vacuum cannot be used, an emergency Cesarean section should be performed.
Malpresentation – if the baby’s head is not presenting properly in the birth canal, this may result in failure of the labor to progress. This can happen when the baby is in breech (the buttocks are in the birth canal instead of the head), face, brow, and compound presentations as well as when the baby is in a transverse lie. Risk factors include multiple pregnancies, previously affected pregnancy, polyhydramnios (too much amniotic fluid, i.e., amniotic fluid index above 18), and fetal and uterine anomalies.26
Macrosomia – The term fetal macrosomia implies fetal growth beyond a specific weight, usually 4,000 g (8 lb, 13 oz) or 4,500 g (9 lb, 4 oz), regardless of the fetal gestational age.In macrosomic infants, the risk of fracture of the clavicular bone in the shoulder and brachial plexus injury is approximately 10-fold and 18- to 21-fold, respectively, when birth weight is more than 4,500 g. The risk of Cesarean delivery in women attempting a vaginal delivery at least doubles when the fetal weight is estimated to be more than 4,500 g.27
Congenital anomaly – Cesarean delivery may improve neonatal outcome for fetuses with isolated brain deformities like meningomyelocele, hydrocephalus with concomitant macrocephaly, anterior wall defects with extracorporeal liver, sacrococcygeal teratomas, hydrops, and alloimmune thrombocytopenia with low platelet count at term. Hydrocephalus without macrocephaly, anterior wall defects without an extracorporeal liver, ovarian cysts, skeletal dysplasias, fetuses whose mothers have immune thrombocytopenic purpura and fetuses with alloimmune thrombocytopenia with acceptable platelet counts may safely be delivered vaginally.28
Abnormal umbilical cord Doppler study – Fetal Doppler flow velocimetry of umbilical and middle cerebral arteries allow for finding of the most proper time of high-risk pregnancy termination, hence should be considered in the elective cesarean sections.29
Thrombocytopenia – this is a condition with low platelet count in the blood and therefore makes the mother more prone to bleeding. Thrombocytopenia is second only to anemia as the most common hematologic abnormality during pregnancy.30
Prior neonatal birth trauma – “Traumatic birth” may refer to physical injury, as well as psychological trauma. In a traumatic birth, it is found that women lose more than just their dream of birth and usually judge themselves to be inadequate in some way. A traumatic birth may arise from the mother’s perceptions in relation to the use of pitocin, forceps, vacuum extraction, and Cesarean section. It can also be related to fear of maternal or fetal death, unrelieved pain during labor and/or childbirth, long and difficult labor, perceived loss of control during the childbirth experience, and a dead or damaged infant.31
Obstetricians must recognize the potential benefits as well as risks of an elective Cesarean section among the birth options for a select group of previously traumatized pregnant women. Although, with support, many women successfully deal with their prior birth trauma, some women, even with therapy, cannot come to terms with it. Therefore it is reasonable to seriously consider their request for an elective Cesarean birth in order to prevent further trauma.32
Risks to the baby during Cesarean section include:
- Breathing problems. Several studies have documented the high incidence of respiratory distress and NICU admissions in infants born by Cesarean delivery before the onset of spontaneous labor.33,34 Babies born by scheduled C section are more likely to develop transient tachypnea — a breathing problem marked by abnormally fast breathing during the first few days after birth.
- Surgical injury.Although rare, accidental nicks to the baby’s skin on the baby’s head, face or whatever part is next to the uterus as the obstetrician is incising the uterus.
Risks to the mother during Cesarean section include:
- Infection.After a C section, the mother might be at risk of developing an infection of the lining of the uterus (endometritis). This can be caused by vaginalbacteria entering the uterus during childbirth and causinginfection within six weeks of the birth (postpartum endometritis). Postpartum endometritis occurs after about 1% to 3% of vaginal births, and up to 27% of cesarean births. Prolonged rupture of the membranes (breaking the bag of water that surrounds the baby) and multiple vaginal examinations during birth also appear to increase the risk.35
- Postpartum hemorrhage (PPH). A C section might cause heavy bleeding during and after delivery. The PPH rate in an emergency Cesarean (6.75%) was greater than after an elective Cesarean (4.84%). Risk factors for PPH after an elective operation include the presence of fibroids or leiomyomata, blood disorders, placenta previa, antepartum bleeding, preterm birth, and general anesthesia. Emergecy Cesarean PPH risk factors included blood disorders, retained placenta, antepartum transfusion, antepartum/intrapartum hemorrhage, placenta previa, general anesthesia, and macrosomia.36
- Reactions to anesthesia.Adverse reactions to any type of anesthesia are possible. Luckily, in spite of an increase in the number of Cesarean sections, the incidence of anesthetic-related complications remains low. This is due primarily to the increasing use of regional anesthesia (spinal and or epidural anesthesia). With spinal anesthesia, spinal headaches may occur, and rarely, infection on the site. General anesthesia, on the other hand, a is associated with a 17-fold increase in complications, in particular, failed endotracheal intubation, aspiration of gastric contents and hypoxia.37
- Blood clots.A C section might increase the risk of developing a blood clot inside a deep vein, especially in the legs or pelvic organs (deep vein thrombosis). If a blood clot travels to the lungs and blocks blood flow (pulmonary embolism), the damage can be life-threatening.
- Wound infection.Depending on the risk factors and whether an emergency C section is needed, one might be at increased risk of an incision infection.
- Surgical injury.Although rare, surgical injuries to the bladder or bowel can occur during a C section. If there is a surgical injury during the C-section, additional surgery might be needed.
- Increased risks during future pregnancies.After a C section, one is faced with a higher risk of potentially serious complications in a subsequent pregnancy than after a vaginal delivery. The more C sections a woman has, the higher the risks of placenta previa and a condition in which the placenta becomes abnormally attached to the wall of the uterus (placenta accreta). The risk of the uterus tearing open along the scar line from a prior C section (uterine rupture) is also higher if a VBAC is attempted.
- Cunningham FG, et al. Williams Obstetrics. 24th Ed. 2014. 587-88.
- Guise JM, McDonagh MS, Osterweil P, Nygren P, Chan BKS, Helfand M. Systematic review of the incidence and consequences
- Declercq E, Barger M, Cabral HJ, et al: Maternal outcomes associated with planned primary cesarean births compared with planned vaginal births. Obstet Gynecol 109(3):669, 2007
- Geller EJ, Wu JM, Jannelli ML, et al: Maternal outcomes associated with planned vaginal versus planned primary cesarean delivery. Am J Perinatol 27(9):675, 2010
- Liu SL, Liston RM, Joseph KS, et al: Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ 176(4):455, 2007
- Glazener C, Elders A, Macarthur C, et al: Childbirth and prolapse: long-term associations with the symptoms and objective measurement of pelvic organ prolapse. BJOG 120(2):161, 2013
- Gyhagen M, Bullarbo M, Nielsen TF, et al: The prevalence of urinary incontinence 20 years after childbirth: a national cohort study in singleton primiparae after vaginal or caesarean delivery. BJOG 120(2):144, 2013
- Handa VL, Blomquist JL, Knoepp LR, et al: Pelvic floor disorders 5–10 years after vaginal or cesarean childbirth. Obstet Gynecol 118(4):777, 2011
- Leijonhufvud A, Lundholm C, Cnattingius S, et al: Risks of stress urinary incontinence and pelvic organ prolapse surgery in relation to mode of childbirth. Am J Obstet Gynecol 204(1):70.e1, 2011
- Rortveit G, Daltveit AK, Hannestad YS, et al: Urinary incontinence after vaginal delivery or cesarean section. N Engl J Med 348(10):900, 2003
- Chauhan SP1,Magann EF,Wiggs CD,Barrilleaux PS,Martin JN Jr. Pregancy after classic cesarean delivery. Obster Gynecol 2002 Nov 100(5 Pt 1):946-50.
- Baron J., Weintraub A. Y., Eshkoli T., Hershkovitz R., and Sheiner E.. 2014.The consequences of previous uterine scar dehiscence and cesarean delivery on subsequent births.Int. J. Gynaecol. Obstet.126:120–122.[PubMed]
- https://www.medscape.com/viewarticle/411928
- Stone KM, Brooks CA, Guinan ME, et al. National surveillance for neonatalHerpes simplexvirus infection.Sex Trans Dis1989;16:152-6.[PubMed]
- Whitley RJ, Corey L, Arvin A, et al. Changing presentation of neonatalHerpes simplexvirus infection.J Infect Dis1988;158:109-16.[PubMed]
- Brown ZA, Wald A, Morrows A, et al. Effect of serologic status and cesarean delivery on transmission rates ofHerpes simplexvirus from mother to infant.JAMA2003;289:203-9.[PubMed]
- Rombaldi RL, et al. Perinatal transmission of human papillomavirus DNA, Virol J, 2009, 6:83.
- Syranjen S. Current concepts on human papillomavirus in children. APMIS, 2010, 118: 494-509
- Armbruster-Moraes E, et al. Presence of human papillomavirus DNA in amniotic fluids of pregnant women with cervical lesion, Gynecol Oncol, 1994, 54:152-8.
- Yap SC, Drenthen W, Pieper PG, et al. On behalf of the ZAHARA Investigators. Risk of complications during pregnancy in women with congenital aortic stenosis.Int J Cardiol.2008;126:240–246. doi: 10.1016/j.ijcard.2007.03.134.[PubMed][Cross Ref]
- Balci A, Drenthen W, Mulder BJ, et al. Pregnancy in women with corrected tetralogy of Fallot: occurrence and predictors of adverse events.Am Heart J.2011;161:307–313. doi: 10.1016/j.ahj.2010.10.027.[PubMed][Cross Ref]
- Regitz-Zagrosek V, Blomstrom Lundqvist C, Borghi C et al. ESC guidelines on the management of cardiovascular diseases during pregnancy of the European Society of Cardiology. Eur Heart J. 2011; Aug 26 (Epub ahead of print; doi:10.1093/eurheartj/ehr218)
- Surapanthapisit P1,Thitadilok W. Risk factors of caesarean section due to cephalopelvic disproportion. J Med Assoc Thai.2006 Oct;89 Suppl 4:S105-11.
- James, A, et al. Failed Operative Vaginal Delivery. Obstet Gynecol. 2009 Nov; 114(5): 1017–1022.
- Sheiner, E, et al. Clinical significance of fetal heart rate tracings during the second stage of labor. Obstet Gynecol 2001 May;97(5 Pt 1):747-52.
- Sharshiner R1,Silver RM.. Management of fetal malpresentation.
Clin Obstet Gynecol2015 Jun;58(2):246-55. doi: 10. 1097/GRF. 0000000000000103. - Chatfield, J. ACOG issues guidelines of fetal macrosomia. Am Fam Physician.2001Jul1;64(1):169-170
- Kuller JA, et al. Cesarean delivery for fetal malformations. Obstet Gynecol Surv. 1996 Jun;51(6):371-5.
- Mizgiert, et al. Fetal flow velocimetry measurements as indications for cesarean section. Ginekol Pol. 1997 Aug;68(8):337-43.
- Sullivan CA, Martin JN., Jr Management of the obstetric patient with thrombocytopenia.Clin Obstet Gynecol.1995;38:521–34.[PubMed]
- Panuthos C, Romero C. 1984.Ended beginnings: Healing childbirth losses. Westport, CT: Greenwood Publishing Corp.
- Patti Spiegelberg Gardner, CNM, MSN. Previous Traumatic Birth: An Impetus for Requested Cesarean Birth. J Perinat Educ. 2003 Winter; 12(1): 1–5. doi:10.1624/105812403X106676
- Zanardo V, Padovani E, Pittini C, et al. The influence of timing of elective cesarean section on risk of neonatal pneumothorax.J Pediatr.2007;150:252.[PubMed]
- Zanardo V, Simbi AK, Franzoi M, et al. Neonatal respiratory morbidity risk and mode of delivery at term: influence of timing of elective caesarean delivery.Acta Paediatr.2004;93:643.[PubMed]
- Mackeen AD, Packard RE, Ota E, Speer L.Antibiotic regimens for postpartum endometritis.Cochrane Database of Systematic Reviews2015, Issue 2. Art. No.: CD001067. DOI: 10.1002/14651858.CD001067.pub3.Link to Cochrane Library. [PubMed]
- https://www.researchgate.net/publication/7652898_Postpartum_Hemorrhage_After_Cesarean_Delivery_An_Analysis_of_Risk_Factors [accessed Jun 24 2018].
- Lynch J,Scholz S. [Anaesthetic-related complications of caesarean section]. [Article in German]. Zentralbl Gynakol.2005 Apr;127(2):91-5.
The Human Papillomavirus & The Cervical Cancer Connection
Rebecca B. Singson, M.D., F.P.O.G.S
Cervical cancer is the most common cancer in the female reproductive system. It is the second most common cancer afflicting females second only to breast cancer. What most people don’t realize is that cervical cancer is now recognized to be the first identified virally induced cancer in women. Research over the last few years has provided overwhelming evidence that infections with a high risk type of cancer-inducing Human papillomavirus (HPV) is necessary for the development of cancer. Understanding what can cause it and knowing how to monitor cervical cancer progression makes it one of the most highly preventable cancers afflicting the female.
Was the Pap Smear Not Doing the Job?
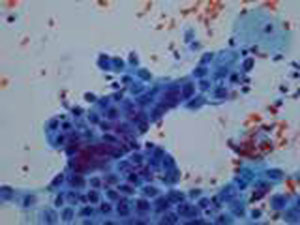
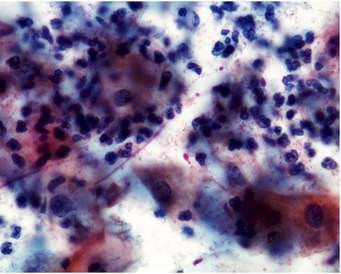
Fig 1. Pap smear under the microscope
There is no doubt that the introduction of cervical cytology introduced by Papanicolau (thus called the Pap smear), had a major impact in bringing about a significant reduction in the incidence of and mortality resulting from cervical cancer in many countries.3 Applying this massive screening program some fifty years ago has resulted in a 50-70% reduction of mortality resulting from cervical cancer. However, even in highly developed countries, this impact has not reached the desired levels expected from implementing a massive screening program because it has not resulted in the eradication of the disease and women are still dying from it.4
A recent critical review of evidence-based data showed that a single Pap smear misses up to 50% of cervical cancer precursor lesions.5 That’s one out of two!! Knowing this makes us now partly understand why cervical cancer continues to occur at such unacceptably high incidence rates, even in countries where the government spends money to subject its population to massive screening.
Understanding What Causes Cervical Cancer: the Viral Connection
Fig. 2. The humanpapillomavirus as seen on electron microscopy
Although the sensitivity of the Pap smear in picking up cervical cancer has not changed much in the last 10 years, there has been rapid growth in our knowledge as to what causes cervical cancer. Research has shown that the human papillomavirus is present in 99.7% of cervical cancers.2
What is this Wart-Causing Human Papillomavirus?
The human papillomavirus (HPV) is a double stranded DNA virus which infects the surface cells lining our tissues called epithelial cells. There are more than 70 distinct site-specific types (meaning they will grow on one part of the body but not on another). Of these, about 35 types are found in the anus and the genital areas, causing warts, also called condylomata acuminata and cervical cancer, the most notorious being types 16 and 18.

Fig. 3. Genital warts or condyloma acuminate caused by the HPV virus.
These infections are considered sexually transmitted and are among the most common sexually transmitted diseases in most countries affecting up to 40% of women with a yearly incidence of 10-15%6 . Many of the HPV infections do not show any signs of symptoms, and are therefore subclinical. It has been found that infections are relatively short-lived lasting usually 8-10 months.7 This indicates that our bodies are indeed capable of clearing the virus which is why in women over 30 years old, the prevalence drops down to 5-10%. Persistent infections, however, are found in 5-10% in women over 35 years old.6 It is in this group of women who are not able to clear the virus from their bodies that cancer in the cervix now has a chance to progress. Research in the last 10 years has consistently detected HPV in more than 90% of cases of cervical cancer, and in some studies, have found it in all cases.
Is There a Way to Test if You are Positive for the Human Papillomavirus?
Because of advances in our knowledge linking the human papillomavirus to the causation of cervical cancer, it became necessary to develop HPV tests that would indicate if the woman was positive for the high-risk strains of the virus that would increase her risk for cervical cancer. The HPV DNA test is a commercially available test which tests for the presence of pieces of the HPV virus. It has has a sensitivity of >90%1 and a negative predictive value of over >90%.
The test entails taking cervical swabs, much like a Pap smear, using the brush from a cervical sampler. Pap smear collected with a broom collection device and rinsed in a solution in a plastic vial collecting system may also be used to provide the same specimen for HPV testing. Pap smears are still done in 2 ways: the conventional way is by smearing the cervical swab on a glass slide; the latest way is to use the broom collection device which immediately washed in a special fluid then run in a machine that filters out the cells from the solution and deposits them in a thin uniform monolayer of cells on a glass slide. The latter has the advantage of eliminating blood and musus from the specimen and makes it easier to examine under the microscope without the debris. The other advantage is that it can also provide the sample to test for HPV testing in case you deem it necessary. So, you can, in fact, ask your gynecologist to perform the test when you get your next Pap smear. Many recent studies have shown that the combination of HPV DNA test and Pap smear improves the detection rate of pre-cancerous lesions of the cervix compared to Pap smear alone.
What Does a Positive HPV Result Mean?
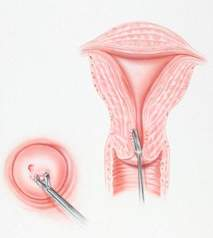
In women over 30, a positive result for high-risk types of HPVDNA means that she has a potentially persistent infection which means that she has a high risk of developing invasive cervical cancer. She should be immediately referred for colposcopy. This procedure involves looking at the cervix under high magnification, applying dyes to visualize abnormal cervical tissue and performing a biopsy, when necessary, of these abnormal areas. Women over 30 years old with a normal Pap smear but test positive for high-risk HPV have a 116-fold risk for developing high grade pre-cancerous lesions of the cervix compared to women who are HPV-negative.
Women in their 20s with a positive HPV DNA result should have a repeat HPV test after 9 months to one year. Since most HPV infections are transient, the virus should normally be cleared in 9 months, particularly in women younger than 30. If the test turns up to be negative, it means the infection has resolved and the woman can be monitored subsequently with Pap smears.
Are There Women Who Are At Increased Risk Than Others?
Since the virus is considered a sexually-transmitted disease, women who started having contact at an age earlier than 18 are at greater risk of acquiring the virus. Women who also have had more than 5 sexual partners or have had partners who have had more than 5 sexual partners are also at increased risk of being HPV positive.
It has been found that women who have had 5 vaginal births or more or have had a pregnancy before 18 yrs. are at increased risk of developing cervical cancer. It is possible that the immune state during pregnancy allows the virus to exert changes in the DNA of the cervical cells, thus, promoting cancer. It has also been found that smoking increases the risk of cervical cancer as well as having a partner who is not circumcised.
If any of the above conditions apply to you, it is best to test for HPV DNA in order to know your risk for developing precursor lesions in the cervix.
Our knowledge of cervical cancer has allowed man to create diagnostic tests that can determine a woman’s risk for developing cervical cancer. We are at an era where cervical cancer is a highly preventable disease. To die from it because we missed the test would be a crying shame.
Treatment
- LEEP – a loop electrosurgical excision procedure may be done to remove cervical lesions in the intra-epithelial stages before it becomes frank cancer. It is a conservative procedure especially for women desirous to preserve their fertility.
- Total hysterectomy – It is another form of management for cervical lesions before it becomes frank cancer. It involves the removal of the cervix and uterus. It may be done through an abdominal incision, transvaginally or minimally invasively using laparoscopic surgery or robotic surgery
- Radical hysterectomy, it is to remove cervix, uterus, upper vagina, ovaries, oviducts and affected lymph nodes. It may be done through open surgery with traditional abdominal incisions or with minimally invasive surgery using tiny, band-aid incisions using the Da Vinci (robotic surgery).
- Radiotherapy includes external radiation exposure and intra-cavitary irradiation. Cervical cancers from different stages can have radiotherapy. It may be a preferred option for patients with frank cancer who cannot tolerate surgery or whose cancer is beyond stage 2-A. It would, however, hurt the ovarian functions of females who undergo this before menopause.
- Chemotherapy for cervical cancer is the used of chemotherapeutic drugs for treatment, which is applicable to the patients from late stage or are suffering from recurrent cervical cancers. The side effects, however, are toxic and the patients may suffer more from that than the disease itself.
REFERENCES:
- National Institutes of Health (NIH) Consensus Development Statement1996.
- Walboomers JMMM, et al. Human papillomavirus, a necessary cause of invasive cervical cancer Worldwide. J Pathol.189:12-19 (1999).
- Hakama M, et al. Effect of organized screening on the risk of cervical cancer in the Nordic countries. In Miller AB, et al (eds.): Cancer Screening. Cambridge, Cambridge University Press, 1991: 153-162.
- Koss LG. The Papanicolau test for cervical cancerT detection: a triumph and a tragedy. JAMA1989; 261:737-43.
- Federal study shows conventional Pap test remains most effective was to diagnose cervical cancer. ACOG Today, March 1999, 43 (3).
- Shah KV, Howley PM Papillomavirus. In: Fields MN, et al, ed. Fields Virology, 3rd edition, Philadelphia: Lippencott Raven, 1988:2077-2109.
- Ho GYF, et al. Natural history of cervicovaginal papillomavirus infection in young women. N Engl J Med 1998; 338: 423-28.
Recurrent Pregnancy Loss
One of the most distressful phenomena that can happen to a couple trying to conceive is a recurrent pregnancy loss (RPL), which can happen to 2-5% of couples. A miscarriage or spontaneous abortion, is defined as the loss of a clinical pregnancy before 20 completed weeks of gestational age (18 weeks after fertilization) or, if gestational age is unknown, the loss of an embryo/fetus of <400 g.1
Pregnancy loss is actually more common than we think since only 30% of all conceptions result in a live birth.2 Many pregnancies fail before we even detect a positive pregnancy test. Many women think they just had delayed menses but actually, it was an undetected miscarriage. Among the pregnancies we recognize clinically approximately 15% of them result in spontaneous abortion, there are many more pregnancies that fail prior to being clinically recognized.
Nearly half of these are unexplained and the other half are due to causes such as, antiphospholipid syndrome, hormonal and metabolic disorders, uterine anomalies and cytogenetic abnormalities. Other etiologies have been proposed but are still considered controversial, such as chronic endometritis, inherited thrombophilias, luteal phase deficiency, and high sperm DNA fragmentation levels.
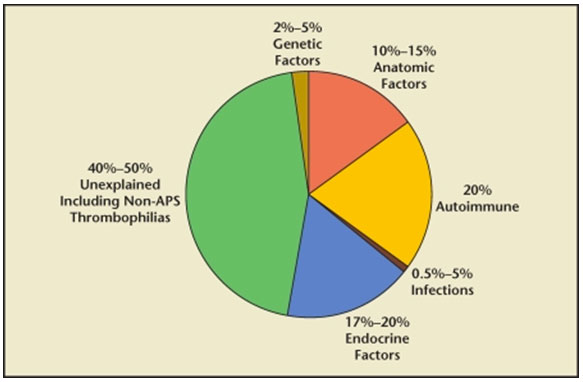
FIG 1. Causes of Infertility.3
ANATOMIC CAUSES
Uterine anomalies are reportedly found in up to 19% of women with RPL and can be classified as acquired or congenital.4
Uterine anomalies are thought to cause miscarriage by interrupting the blood supply of the endometrium, resulting in abnormal placental development. Among the congenital anomalies, the presence a septum in the cavity of the uterus is the one of the most notorious in causing as much as a 76% risk of spontaneous pregnancy loss among affected patients.5 Other uterine anomalies, like the unicornuate, didelphic, and bicornuate uteri have been found to cause less risk for recurrent pregnancy loss.6 Asherman’s Syndrome, or intrauterine adhesions/scarring or synechiae, is an acquired uterine condition, when the front and the back walls of the uterine cavity stick to the each other resulting from overcurettage in evacuating a pregnancy after a miscarriage or after an infection in the lining of the uterus, called endometritis. This may also result in recurrent pregnancy loss. Myoma, a benign tumor in the muscle of the uterus, also called fibroids, if located inside the cavity of the uterus or if located in the muscle of the uterus and are larger than 5 cm, can also cause recurrent pregnancy loss by competing for the blood supply needed for implantation.7
HORMONAL/ENDOCRINOLOGIC CAUSES
Among the endocrinologic disorders implicated in recurrent pregnancy loss, approximately 17% to 20% are found to be due to luteal phase defect (LPD), polycystic ovarian syndrome (PCOS), diabetes mellitus, thyroid disease, and hyperprolactinemia. 8,9
Polycystic Ovary Syndrome has been found in at least 40% of women with RPL 10 , as well as poorly controlled type 1 diabetes.11 The fact that patients improve and miscarry less when on an insulin sensitizing drug, metformin, leads to the theory that insulin resistance and the resultant hyperinsulinemia that is often present in cases of PCOS and type II diabetes mellitus might be a mechanism responsible for causing recurrent pregnancy loss in these patients.12
Hypothyroidism has been associated with spontaneous abortion and RPL.13 but even patients with normal thyroid levels but with antithyroid antibodies have been found to become hypothyroid soon after they get pregnant.14 Pregnancy outcomes in these women may improve with early (possibly prenatal) thyroid hormone replacement.15 The most commonly used criteria to define subclinical hypothyroidism is a serum thyroid-stimulating hormone (TSH) threshold of >2.5 mIU/L. 16
Uncontrolled diabetes has been shown to increase the risk of miscarriage, whereas maintaining good control of sugar before attempting to get pregnant significantly shinks the risk back to normal.17,18
Progesterone deficiency or Luteal Phase Defects, because of its effect on the endometrium in the second half of the menstrual cycle after ovulation happens, called the luteal phase, can impair normal implantation. Many mechanisms, such as inadequate follicular growth, dysfunctional ovulation, poor corpus luteum function, and abnormal endometrial response and receptivity, have been proposed.19,20
Elevated prolactin hormone levels have been found to cause infertility and RPL. altering the hormonal balance and feedback mechanisms involving the hypothalamic–pituitary–ovarian axis, which can lead to impaired formation of eggs in the ovary and failure to ovulate.21
IMMUNOLOGIC CAUSES
As human beings, we are equipped with an immunologic system that protects us from getting ill when invaded by foreign proteins, viruses and bacteria. If you think about it, the fetus is actually a foreign protein with a different genetic material from the mother. How is it then that a pregnancy woman is able to tolerate a foreign protein to grow inside her? That’s because there are many mechanisms and alterations in our immune system to allow us to carry a foreign protein with a different genetic make-up inside our bodies. When some of these mechanisms fail, it also results in failure to implant or to carry the baby to term. One specific auto-immune disorder leading to recurrent pregnancy loss is the Anti-phosopholipid antibody syndrome (APS). It is prevalent in 3% to 5% in the general population and is characterized by the presence of at least 1 clinical and 1 laboratory criterion.22
Diagnostic criteria for APS according to “the International consensus statement on an update of the classification criteria for definite antiphospholipid syndrome”:
| At least 1 clinical and 1 laboratory criteria must be present for definite APS |
|
|---|---|
| Clinical criteria |
|
| I – Vascular thrombosis |
One or more clinical episodes of an arterial, venous, or small vessel thrombosis, in any tissue or organ. Thrombosis must be confirmed by imaging or Doppler studies or |
| histopathology, with the exception of superficial venous thrombosis. For histopathologic confirmation, thrombosis should be without significant evidence of inflammation in the vessel wall. |
|
| II – Obstetric morbidity |
1) One or more unexplained demise of a morphologically normal fetus at or beyond 10 weeks of gestation, with normal fetal morphology documented by ultrasound or by direct examination, or 2) One or more premature births of a morphologically normal neonate before the 34th week of gestation, because of a) eclampsia or severe preeclampsia or b) placental insufficiency, or 3) Three or more unexplained consecutive miscarriages of <10 weeks of gestation. Known factors associated with recurrent miscarriage, including parental genetic, anatomic, and endocrinologic factors should be ruled out. |
| Laboratory criteria |
I – aCL (IgG and/or IgM) in the blood, present in medium or high titers (> 40 GPL or MPL or >99th percentile), on two or more occasions, at least 12 weeks apart, measured by a standardized ELISA. II – Anti-β2GP1 antibody of IgG and/or IgM isotype in the blood (>99th percentile) on two or more occasions, at least 12 weeks apart, measured by a standardized ELISA. III – Lupus anticoagulant present in plasma, on two or more occasions at least 12 weeks apart, detected according to the guidelines of the International Society on Thrombosis and Hemostasis. |
Abbreviations: APS, antiphospholipid syndrome; aCL, anticardiolipin antibody; ELISA, enzyme-linked immunosorbent assay.
LIFESTYLE FACTORS
Several lifestyle factors have been associated with an increased risk of miscarriage: Obesity, defined as a body mass index >30 kg/m2,23,24 smoking,25 excessive caffeine consumption (>300 mg/day, or the equivalent of two cups), excessive alcohol intake,25,26 and cocaine.27 Patients with recurrent pregnancy loss should be advised to modify their lifestyle to avoid these factors.
Genetic factors
The vast majority of early pregnancy losses (50%–60%) are the consequence of chromosomal abnormalities, which can be inherited from either parental, or arise spontaneously in the embryo from parents with normal chromosomes.28.29
Because of the principle of survival of the fittest and natural selection, up to 90% of embryos which contain any abnormal chromosomes are spontaneously aborted. The most commonly found abnormalities are numeric chromosome errors, such as trisomy, polyploidy, and monosomy X. The risk of aneuploidy significantly increases with maternal age.17,28,30,
DIAGNOSIS AND TREATMENT:
It is not recommended to evaluate a couple following one miscarriage.31
it is acceptable to start a workup following two consecutive losses, especially in women aged >35 years.17,31
A thorough gynecologic history should be obtained, as well as a family history of infertility or miscarriage. Both partners should also be questioned about the modifiable lifestyle factors, such a smoking, alcohol use, and nutritional habits as well as presence of genetic problems in the family.17,31,32,33
Diagnostic evaluation for uterine anatomic anomalies should include office hysteroscopy or hysterosalpingography (HSG). Hysteroscopic resection of intrauterine adhesions and intrauterine septa are indicated if these abnormalities are identified. Patients undergoing successful hysteroscopic septum resection seem to enjoy near normal pregnancy outcomes, with term delivery rates of approximately 75% and live birth rates approximating 85%.34 Myomectomy should be considered in cases of submucosal fibroids or any type fibroids larger than 5 cm. Resection has been shown to significantly improve live birth rates from 57% to 93%.35 Depending on the size and location, myomectomy can be performed via the following modalities: robotic surgery, laparoscopy, open laparotomy, or hysteroscopy.
For APAS patients with RPL, tests for anticardiolipin antibodies and lupus anticoagulant should be included. Treatment should include low-dose aspirin (LDA, 81–100 mg/d) plus prophylactic low-molecular-weight heparin in otherwise healthy women without a history of of a systemic autoimmune disease such as systemic lupus erythematosus, or a history of thrombosis. Low dose aspirin
should be started before conception or with a positive pregnancy test. Heparin treatment should be started with a positive pregnancy test.36 Heparin is a large complex of molecules that do not cross the placenta and, as such, is regarded as safe during pregnancy.
For endocrine evaluation, prolactin levels can be tested three hours from waking up, thyroid hormones without any preparation. For women with elevated prolactin levels, called hyperprolactinemia and RPL, treatment with drugs like bromocriptine 2.5–5 mg/day until 9th week of gestation, significantly decreased miscarriage rates compared to no treatment.37
For cases of Polycystic ovary, the diagnosis is clinched with the presence of two out of three criteria: 1. irregular menses, 2. evidence of high levels of testosterone like hirsutism, acne or elevated testosterone hormone level; 3. Polycystic ovaries by ultrasound. Therapy involves weight management, when overweight or obese, and giving with insulin sensitizing drugs like metformin, and progesterone treatment. Other relevant tests may be a Thyroid-stimulating Hormone evaluation, Anti-Mullerian hormone evaluation to check for ovarian reserve, serum prolactin in patients with irregular menses, anti-thyroid antibody testing and endometrial biopsy when indicated, to evaluation luteal phase defects.
For luteal phase defects, Progesterone supplementation is the most widely used treatment because of its availability, ease of administration, and tolerability.
UNEXPLAINED RECURRENT PREGNANCY LOSS
Despite all the work-up, almost half of patients will remain without a definitive diagnosis and unexplained causes. It remains unclear how to best manage these patients although Progesterone treatment has been found to be of benefit in decreasing the miscarriage rate among women who have experienced at least 3 losses.38 Low-dose aspirin has also been investigated as a potential therapy for unexplained RPL. Its use prior to and during pregnancy has only been proven to increase live birth rates among those women with previous miscarriages beyond 13 weeks of gestation.39,40
ON A POSITIVE NOTE
Despite the depression that couples feel after recurrent pregnancy losses, it might help to focus on the fact that there is still a high probability of success on a subsequent pregnancy. it can be helpful for the physician and patient to keep in mind the relatively high likelihood that the next pregnancy will be successful. Overall, the prognosis for RPL is encouraging. Even with the diagnosis of RPL and as many as 4 to 5 prior losses, a patient has a greater than 60% to 65% chance of carrying her next pregnancy to term.41
- Zegers-Hochschild F, Adamson GD, de Mouzon J, et al. International Committee for Monitoring Assisted Reproductive Technology; World Health Organization. International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary of ART terminology, 2009. Fertil Steril. 2009;92(5):1520–1524. [PubMed]
- Macklon NS, Geraedts JPM, Fauser BCJM. Conception to ongoing pregnancy: the “black box” of early pregnancy loss. Hum Reprod Update. 2002;8:333–343. [PubMed]
- Ford HB, Shust DJ. Recurrent Pregnancy loss: Etiology, Diagnosis & Therapy. Rev Obstet Gynecol. 2009 Spring; 2(2): 76–83.
- Jaslow CR, Carney JL, Kutteh WH. Diagnostic factors identified in 1020 women with two versus three or more recurrent pregnancy losses. Fertil Steril. 2010;93(4):1234–1243. [PubMed]
- Raga F, Bauset C, Remohi J, et al. Reproductive impact of congenital Müllerian anomalies. Hum Reprod. 1997;12:2277–2281. [PubMed]
- Lin PC. Reproductive outcomes in women with uterine anomalies. J Womens Health. 2004;13:33–39.[PubMed]
- Bajekal N, Li TC. Fibroids, infertility and pregnancy wastage. Hum Reprod Update. 2000;6:614–620.[PubMed]
- Stephenson MD. Frequency of factors associated with habitual abortion in 197 couples. Fertil Steril.1996;66:24–29. [PubMed]
- Fox-Lee L, Schust DJ. Recurrent pregnancy loss. In: Berek JS, editor. Berek and Novak’s Gynecology.Philadelphia: Lippincott Williams & Wilkins; 2007. pp. 1277–1322.
- Rai R, Backos M, Rushworth F, Regan L. Polycystic ovaries and recurrent miscarriage—a reappraisal.Hum Reprod. 2000;15:612–615. [PubMed]
- Mills JL, Simpson JL, Driscoll SG, et al. Incidence of spontaneous abortion among normal women and insulin-dependent diabetic women whose pregnancies were identified within 21 days of conception. N Engl J Med. 1988;319:1617–1623. [PubMed]
- Glueck CJ, Wang P, Goldenberg N, Sieve-Smith L. Pregnancy outcomes among women with polycystic ovary syndrome treated with metformin. Hum Reprod. 2002;17:2858–2864. [PubMed]
- Vaquero E, Lazzarin N, De Carolis H, et al. Mild thyroid abnormalities and recurrent spontaneous abortion: diagnostic and therapeutical approach. Am J Reprod Immunol. 2000;43:204–208. [PubMed]
- Poppe K, Velkeniers B, Glinoer D. The role of thyroid autoimmunity in fertility and pregnancy. Nat Clin Pract Endocrinol Metab. 2008;4:394–405. [PubMed]
- Negro R, Formoso G, Coppola L, et al. Euthyroid women with autoimmune disease undergoing assisted reproduction technologies: the role of autoimmune disease and thyroid function. J Endocrinol Invest. 2007;30:3–8. [PubMed]
- De Groot L, Abalovich M, Alexander EK, et al. Management of thyroid dysfunction during pregnancy and postpartum: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab.2012;97(8):2543–2565. [PubMed]
- Practice Committee of the American Society for Reproductive Medicine Evaluation and treatment of recurrent pregnancy loss: a committee opinion. Fertil Steril. 2012;98(5):1103–1111. [PubMed]
- Jovanovic L, Knopp H, Kim H, et al. Elevated pregnancy losses at high and low extremes of maternal glucose in early normal and diabetic pregnancies: evidence for a protective adaptation in diabetes. Diabetes Care. 2005;28(5):1113–1117. [PubMed]
- Jones GS. The luteal phase defect. Fertil Steril. 1976;27(4):351–356. [PubMed]
- Li TC, Spuijbroek MD, Tuckerman E, et al. Endocrinological and endometrial factors in recurrent miscarriage. BJOG. 2000;107(12):1471–1479. [PubMed]
- Bussen S, Sütterlin M, Steck T. Endocrine abnormalities during the follicular phase in women with recurrent spontaneous abortion. Hum Reprod. 1999;14(1):18–20. [PubMed]
- Derksen RHWM. The obstetric antiphospholipid syndrome. J Reprod Immunol. 2008;77:41–50.[PubMed]
VAGINAL DRYNESS
WHAT IS VAGINAL DRYNESS? WHY DOES IT OCCUR?
It is the sensation a woman gets when there is not enough moistness or lubrication in the vagina. It occurs when when there are hormonal changes like after childbirth, during breastfeeding or while on birth control pills. Prescription medicines with anticholinergic or sympathomimetic effects such as anti-allergy drugs, cardiovascular or psychiatric drugs also dry out not only the mucosal lining or wet tissue of the mouth but also that of the vagina. Through a simone is anxious or stressed, or
WHAT IS ITS RELATION TO MENOPAUSE?
What happens in menopause is the ovaries cease to function and the estrogen and progesterone hormones begin to drop. As a result, the lining of the vagina thins our from about 8 layers of cells to 3 layers, losing elasticity and capacity to produce fluid.
WHAT ARE THE PHYSICAL, EMOTIONAL AND PSYCHOLOGICAL EFFECTS OF VAGINAL DRYNESS
Vaginal dryness can cause painful intercourse which can certainly affect the degree of pleasure with sex. Many women undergoing stress, anxiety or menopause who experience painful intercourse will naturally want to avoid sex. This can lead to a feeling of rejection of the spouse and cause a strain on the relationship.
HOW CAN IT BE TREATED?
If the cause is stress or anxiety, removal of the stressful situation may relieve the problem. Discontinuance of medications that cause the dryness will usually reverse the dryness. Hormone replacement therapy in the form of estrogen progesterone pills can cause the lining of the vagina to thicken and become more lubricated again.. Vaginal estrogen tablets can also act locally to achieve the same effect. For those who refuse hormonal therapy may relieve the dryness with vaginal lubricants.
WHAT ARE THE SIDE EFFECTS IN USING LUBRICANTS AND VAGINAL MOISTURIZERS? WHAT SHOULD CONSUMERS LOOK FOR IN CHOOSING THE RIGHT PRODUCT TO USE?
It is important to avoid using Petroleum based lubricants like Vaseline or even baby oil since these can promote infections. Use only water-soluble lubricants with glycerine which are odorless, tasteless and sterile. KY Jelly is the most available in any drugstore nationwide. In the U.S. Astroglide and Replens are also available. In the Philippines, among the brands available are Felina and Replens. Some lubricants which may contain a spermicidal, Nonoxynol may cause vaginal irritation because of the latter.
HAVE YOU HAD PATIENTS WITH VAGINAL DRYNESS? IS IT ALSO A COMMON PROBLEM AMONG FILIPINAS? WHAT ARE THEIR USUAL COMPLAINT?
Many patients especially those in menopause who are not on hormone replacement therapy complain of vaginal dryness. They usually complain of painful intercourse and when you ask them if it is upon entry or on deep penetration, they usually answer, “upon entry”. Then you elicit for vaginal dryness and they admit they do. Some of them actually come for consultation.primarily for that problem.
WHAT IS THE PREVAILING ATTITUDE OF WOMEN WITH REGARDS TO THIS CONDITION. ARE THEY OPEN ABOUT IT? DO THEY ALSO DISCUSS IS WITH THEIR SPOUSES?
Women whose husbands have a medical problem that prevents him from being sexual are not bothered at all with vaginal dryness. It is among those with sexually active husbands that vaginal dryness becomes a major concern. These women are open about it with their gynecologists knowing they can be helped. They can’t deny it to their spouses since intercourse becomes difficult. Most of them can discuss it with their spouses and the usual resolution is the use of KY Jelly.
HOW TO AVOID PAINFUL SEX THE FIRST TIME AROUND
Dr. Rebecca B. Singson, FPOGS, FACS, FPSCPC, LMT
Athough statistics show that one third of our youth are already engaging in pre-marital sex, there are still the two thirds who approach marriage keeping their virginity intact. There are still women who value their virginity as something they would reserve for their spouse.
Whether done premaritally or with the blessings of marriage, first time intercourse is approached with mixed reactions of anxiety, excitement, arousal and even fear. What can be done to make it as least traumatic as possible?
WHAT IS DYSPAREUNIA?
Dyspareunia (“dis-par-oon-ya”) is painful sex, due to medical or psychological reasons. It is used mostly to describe women, although men can also suffer pain during sexual contact. Most of the time, the cause can be reversed, even when long-standing, but for some, it may be a recurrent ordeal. When pain occurs, the woman experiencing dyspareunia may be distracted from feeling pleasure and excitement. Both vaginal lubrication and vaginal dilation decrease and she may begin to have a negative association with sex just anticipating the pain.
WHAT ARE THE CAUSES?
Pain during sex may happen in any part of the genitals. It is important to differentiate whether the pain happens upon penetration or on deep penetration or if it happens way after intercourse is over, because the causes may be entirely different.
Superficial dyspareunia is pain upon entry. The pain from these conditions is usually felt when a tampon or penis is inserted into the vagina. Sometimes, even sitting or wearing pants can cause discomfort. The most common cause of painful entry is lack of lubrication from lack of foreplay where the woman has not been “warmed up” by her partner and has, therefore, not been lubricated well enough. A man can reach his orgasm in 2 mins. but for a woman, it is prudent to spend at least 20 mins. on foreplay and insure the female genitals are well-flooded before entry begins. In pre-menopausal or menopausal women, this can be real concern because when estrogen wanes during this time of the woman’s life, the vulvar and vaginal skin thins out, dries out, and produces less lubrication which comes from transudation through the vaginal skin.
Dermatologic conditions can also cause pain upon entry. Sometimes it can be caused by something as simple as using soap to wash the external genitals or using the wrong vaginal wash. Frequent douching or washing especially with soaps or the wrong vaginal wash can kill the good bacteria or cause allergies from the chemicals used. Most soaps (even the mildest such as baby soap or Ivory or Dove) have a ph of 7 and above, meaning it has an alkaline ph. That is appropriate to cleanse the skin of the rest of the body but the female genitals need to maintain a ph of 3.5-5.5 to keep alive the protective bacteria, the lactobacilli, and doing their job of protecting you from fungal and bacterial infections. Tipping off the ph can make you prone to yeast infections or to bacterial vaginosis which can manifest with a discharge, a foul smell (more typical with bacterial vaginosis described as “fishy odor”) and skin irritation. This is the reason vaginal washes were produced to keep the vagina at the appropriate ph. However, not all vaginal washes are created alike. Some are more irritating than others because of the chemicals used to disinfect, color or perfume the solution. It is best to stick to lactic acid-based washes.
A viral infection such as Herpes can also produce painful sores on the genitals, both for males and females that can be transmitted to an uninfected partner, aside from increasing your predisposition to fungal infections. An infection of the Bartholin’s gland at the opening of the vaginal may produce a swelling or inflammation that may make entry during sex painful. A scar tissue from a previous episiotomy (cut on the perineum during a normal birth) can also cause pain during intercourse.
Vulvar Vestibulitis Syndrome (VVS) is the most common subtype of vulvodynia (medical term meaning chronic vulvar discomfort e.g. burning, stinging, irritation, rawness). affecting premenopausal women. It tends to be associated with a highly localized “burning” or “cutting” type of pain. The woman senses the irritation and burning which can be felt hours or days after sex, giving one a sense of hopelessness and depression (Bergeron et al. 1997; Marinoff and Turner 1991;[2] Peckham et al. 1986).
The prevalence of VVS is quite high: affecting 10%-15% of women seeking gynecological care (Bergeron et al. 1997). You can feel severe pain at the opening of the vagina with attempted penetration and after penetration you become sore and tender with pressure. Your doctor can apply the cotton-swab test, in which pressure is applied in a circular fashion around the vulvar vestibule to assess complaints of pain. The causes may include a subclinical human papillomavirus infection, chronic recurrent candidiasis, or chronic recurrent bacterial vaginosis (Marinoff and Turner 1991; Peckham et al. 1986) or it could result from chronic hypertonic perivaginal muscles, leading to vaginal tightening and subsequent pain. Some researchers even believe there is a neurological cause to it relating to thickened changes of the nerves. Finally, psychological factors may even worsen the problem, because the moment you think or desire sex upon arousal, it causes you to anticipate the pain, thus resulting in a conditioned spasmodic reflex . Problems with your spouse then emerge with chronic frustration, disappointment, and depression along with it.
Deep dyspareunia is pain on deep penetration or deep thrusting can be caused by a chronic pelvic inflammatory disease such as gonorrhea or Chlamydia or by endometriosis (condition where the lining of the uterus implants outside the uterus so everytime you menstruate, you bleed into the abdominal cavity). Pelvic masses such as myomas or ovarian cysts can also cause pain.
Vaginismus (“vag-in-is-mus”) is a spasm of the muscles around the vagina, sometimes so severe that penile penetration is impossible. Causes can be from past sexual abuse, painful 1st sexual intercourse or gynecologic examination, religious brainwashing to think that sex is “bad or dirty” or a misconception in the size of the vagina, an unopened hymen (yes, anatomic defect where there is no hole), chronic infection like gonorrhea or Chlamydia.
Interstitial Cystitis (IC). is now a recognized cause of dyspareunia. It is a condition where patients may struggle with bladder pain and discomfort during or after sex. For women with IC, pain usually occurs the following day, the result of painful, spasmodic contractions of the pelvic floor muscles. Men are not spared from this condition since pain occurs at the moment of ejaculation and is focused at the tip of the penis. Interstitial cystitis patients also struggle with urinary frequency and/or urinary urgency.
Dyspareunia in Men
In men, as in women, there are a number of physical factors that may cause sexual discomfort. Sometimes, immediatlely after ejacuation, pain is experienced in the testicular or glans area of the penis. This may be caused by infections of the prostate, bladder, or seminal vesicles can lead to post-ejaculatory intense burning or itching. Men suffering from interstitial cystitis and gonorrhea may also experience intense pain at the moment of ejaculation. Urethritis or prostatitis can likewise make genital stimulation painful or uncomfortable. Anatomic deformities of the penis such as Peyronie’s disease should also be ruled out since it may also result in pain during coitus. One not-so-obvious cause of painful intercourse may be the painful retraction of a too-tight foreskin, occurring either during the first attempt at intercourse or subsequent to tightening or scarring following inflammation or local infection (Bancroft 1989). During vigorous intercourse or masturbation, small tears may occur in the frenulum of the foreskin and can be very painful.
A rare form of male dyspareunia – postejaculatory pain syndrome – manifests with persistent and recurring pain described as sharp, stabbing and/or burning, in the genital organs during ejaculation or immediately thereafter. Although the pain lasts only briefly, it can persist and be quite intense. Although the immediate cause of this psychogenic problem is the involuntary painful spasm or cramping of certain pain-sensitive muscles in the male genital and reproductive organs, the excruciatingly painful muscle cramps may be attributable to a man’s conflict about ejaculating.
A pelvic floor disorder can also be the cause of pain during and after sex. Spasmodic, inflammed, overtoned or shortened pelvic muscles can result in the compression or sometimes the entrapment of the pudendal nerve, the nerve supplying the pelvic floor.
Guilt about sexual pleasure or about the paraphiliac nature(a sexual deviation where sexual fantasies revolve around a non-human object or a non-consenting partner like a child, or involving pain or humiliation of self or partner) of the erotic fantasies can lead to pain with orgasm. In other cases, men who want sexual freedom but is with a sexually inhibited partner may feel general resentment, or be angry at their current sexual partners for unconscious or conscious reasons.
WHAT CAN BE DONE
Seek counsel with your obstetrician who can differentiate the diagnosis based on your symptoms.Your Ob-gyn must elicit a complete history and perform a physical exam to determine where is the exact pain, what triggers it and timing of the pain. For dypareunia due to lack of lubrication, lubricants abound in the market (Felina, Astroglide and Replens are recommended brands). Bartholin Duct cysts can be excised. Laboratory tests to exclude fungal, bacterial or viral infection must be done. It atrophy of the skin seems to be the cause, hormone replacement therapy is available either orally, transdermally or even locally with vaginal tablets. For deep dyspareunia, an ultrasound or CT scan may clinch the diagnosis. Tumors may be removed surgically and endometriosis may be removed surgically or medically depending on size and extent. Management of psychiatric causes is the most challenging because sex therapists do not abound although the problem of sexual dysfunction does. However, whatever the cause is, professional help is necessary to alleviate the problem of painful intercourse. Admitting it and resolving to seek consult for it can be the first step to an improved sex life and a more wholesome relationship.
IT’S COOL TO STAY A VIRGIN!!
By: REBECCA B. SINGSON, M.D, FPOGS
Let’s face it! Our teens are having sex. According to the 2002 Young Adult Fertility and Sexuality Study by the University of the Philippines Population Institute (UPPI) and the Demographic Research and Development Foundation, twenty-six percent (26%) of our Filipino youth nationwide from ages 15 to 25 admitted to having a pre-marital sex experience. What’s worse is that 38% of our youth are already in a live-in arrangement.
What most young men and women don’t realize is that there are scientific reasons why it’s better to preserve your virginity. Unless you’re completely sure that the benefits far outweigh the risks in getting intimate with your special someone, it’s cool to stay a virgin because:
1) YOU MINIMIZE YOUR RISKS FOR ACQUIRING CERVICAL CANCER
The Human Papillomavirus (HPV) is a sexually-transmitted, wart-forming virus that has been implicated in causing cancer of the cervix. This is the most common cancer in women secondary to breast cancer. Women who are at increased risk for acquiring this are those who engage in sex before 18, have a pregnancy at or younger than 18, or have had at least 5 sexual partners, or have had a partner with at least 5 sexual partners. If you start sex at an early age, you have a higher likelihood of going through several sexual partners before you settle down, thus increasing your exposure to acquiring the virus and acquiring cervical cancer. The men can get genital warts from this virus and can certainly pass it on to their partners, thus increasing her risk for cervical cancer. Is that something you would want to gift to your wife with on your honeymoon? There is a way to test women (HPV Digene test) but no test for the man so you can’t know if you have it. Using the condom does not confer protection against acquiring this virus since the condom cannot cover the testes where the warts can grow and proliferate.
2) YOU MINIMIZE YOUR RISK FOR UNWANTED PREGNANCIES
The 1998 National Demographic and Health Survey (NDHS) reveals that 3.6 million of our teenagers (that’s a whopping 5.2% of our population!) got pregnant. In 92% of these teens, the pregnancy was unplanned, and the majority 78% did not even use contraceptives the first time they had sex. Many of the youth are clueless that even on a single intercourse, they could wind up pregnant.
3) YOU MINIMIZE YOUR RISK FOR FETAL DEATHS
The youth should know that the statistics of the Department of Health (DOH) show that fetal deaths are more likely to happen to young mothers, and that babies born by them are likely to have low birth weight. Those are not the likely circumstances you would like to start your family with.
4) YOU MINIMIZE YOUR POSSIBILITY FOR AN ABORTION
Abortion is illegal in the Philippines yet our rate of abortion here is 25 abortions per 1000 women. It would shock you to know that we even have a higher abortion rate compared to the U.S. where abortion is legal at a rate of 23/1000 women. Unplanned pregnancies lead to abortions. In our country, backdoor abortions are resorted to with untrained “hilots” with questionable sterility procedures, increasing the possibility for tetanus poisoning and other complications.
5) YOU MINIMIZE YOUR RISK FOR ACQUIRING SEXUALLY TRANSMITTED DISEASES
Research shows that boys practice more casual sex or have multiple sex partners and are having sex with commercial sex workers. Once infected, they are likely to be agents in spreading sexually transmitted disease (STD). In general, sex among adolescents is unprotected. Ninety percent (90%) of sexual encounters of males are unprotected. Even their sexual encounters with commercial sex workers are also unprotected (78%). It is essential to realize that according to the Center for Disease Control in the U.S (CDC), three fourths of the women and half of the men infected with Chlamydia have no symptoms at all. Majority of men and women infected with gonorrhea have no symptoms either. And if you think that using the condom gives keeps you safe from STDs. You’re wrong! The condom can protect you from gonorrhea and AIDS but cannot completely protect you from acquiring Chlamydia, herpes and the human papillomavirus, syphilis, and chancroid. The surest way to avoid transmission of sexually transmitted diseases is to abstain from sexual intercourse, or to be in a long-term mutually monogamous relationship with a partner who has been tested and you know is uninfected.
6) YOU DON’T RUN THE RISK OF GETTING PSYCHOLOGICALLY DAMAGED
Once a couple begins to have intercourse, the dynamics of their relationship may change for the better, in terms of increased erotic pleasure and feelings of closeness. However, it may also change for the worse if the woman experiences pain and develops sexual dysfunction which can damage her for life. Feelings about the loss of virginity can be very complex especially in the context of a conservative and orthodox religious background. Men and women who hear stories from their peers may have preconceived notions about how great and pleasurable sex is. When they find out that their own experience is not as they imagined because they experienced less pleasure or are not achieving multiple orgasms, they may end up devaluing sex, their partners, male-female relationships and/or their self esteem may suffer. Even a so called “good” sexual relationship can be detrimental to the process of sexual unfolding because young men may become confused about the meaning of sex in their lives because their early sexual experiences where forced upon them by a more experienced female. They may end up being overwhelmed by their sexual experience, become fearful of female demands and become unsure of the male role in a heterosexual relationship.
7) YOU DON’T RUN THE RISK OF AN EMOTIONAL DISASTER
How many of our youth have lost their scholarship, flunked their exams or worse, become suicidal because they were dumped after having an intense, intimate relationship with someone they gave up their virginity for? There is less at stake when you decide to call it quits if the degree of intimacy has not reached the level of intercourse. It is vital to create a firm idea of who the self is before you can achieve psychosexual maturity. Sexual unfolding is a process that would always be consistent with the emotional maturity. For most, it would require a very gradual experience over many years requiring deliberation, self-discovery and exposure to and creating differential perceptions of other people. In short, collect and collect (friends and suitors) before you select (your mate). Never force the butterfly prematurely out of its cocoon or it will appear with crumpled wings and be crippled to fly for life.
The sexual revolution has ushered in a period in which the average adolescent experiences tremendous pressures to have sexual experience of all kinds. Not only the youth feel pressured but the older virgins also feel apologetic for being a virgin at, let’s say 30 or 40 years old. They suffer from the “virginity burden” syndrome feeling that they are still virgins beyond the “usual” time symbolizing a failure to be appropriately sexual. They equate that to mean that they are not as “normal” or as “free” as other non-virgins so virginity becomes a source of embarrassment.
In this era of AIDS which can lead to death, HPV which can lead to cervical cancer, and unwanted pregnancies, it’s really a cool decision to stay a virgin for all the scientific, psychological and emotional reasons
SEX EDUCATION STARTS AT HOME!!
REBECCA B. SINGSON, MD, FPOGS, FACS, FPSCPC
Little do you know that since the day your kids are born, you are already sending them messages about their sexuality. You dress them in pink to signify they are a girl and blue if they are a boy. Being held and touched, kissed and hugged, snuggled and tickled allows babies to experience comforting, positive physical sensations associated with being loved. The unique type of physical intimacy and emotional attachment between parent and infant can be the early foundation of more mature forms of physical intimacy and love that develop later as part of mature sexuality.The way you touch and cuddle, snuggle, tickle and kiss them lets them experience comforting and positive physical sensations which makes them know they are loved by you. The input you give, the family experiences you create from day one of life will determine whether your child will develop a healthy and positive sexual attitude.
Through your words, as well as your silence, your verbal and non-verbal responses and reactions teach your child your values and attitudes about sexuality.
Getting to know the Body.
Children need to be taught the right labels for their body parts. A penis is the correct word for the boy’s male organ, and the vagina is the correct label for the female sex organ. When you give camouflage names for the sexual body parts, you are conveying the message that there is something wrong or unmentionable or embarrassing about them. The children therefore are quick to absorb the idea that their genitals are something to be ashamed of.
Infants and toddlers naturally touch their genitals during diaper changes or their baby boys have frequent erections. They are curious what lies underneath their clothes and enjoy running around naked. Your verbal and non-verbal reactions with (facial expressions and body language) is what gives your child’s first lessons in sexuality. If you show disapproval with anger, surprise, embarrassment, you teach your child that this curiosity about his or her body is very abnormal, when in fact, it should be a normal part of life.
If your child comes home calling his male organ some word he heard from others like “birdie” or “ wee wee”, you can say, “Some people call it that, but that’s just a made up word. The real name is penis (or vagina as the case may be.)
Children may also be curious about seeing a brother, sister, mother or father in the shower and this is usually how they learn about physical differences between boys and girls.
Identifying Male from Female
By age 2 or 3, a child starts to develop gender identity. This awareness is what gives them the sense of being a male or female. At this age, a toddler starts to understand the difference between boys and girls, and can identify himself or herself as one or the other. Gender identity is biologically determined by the presence or absence of the Y chromosome but to a certain extent, it may also be the product of a child’s environment.
Kids at this age also learn cultural behaviors begin to associate certain behaviors associated with being male or female, called gender roles. We teach them that girls play with dolls and boys play with trucks and planes and cars and guns. Our culture dictates what is masculine or what is feminine, how boys behave versus girls. However, much has changed in society about gender roles because women are becoming pilots, car racers and truck drivers. More and more men are participating in child rearing which was once a mother’s turf, and some are role reversing with the fathers as “housebands” and wives going out to work. Therefore, it’s ok for boys to play with dolls and for girls to play with the boy’s toys so you don’t stereotype sexes into limited roles. Be sensitive as well to use the word “firefighter” instead of “fireman” and “chairperson” instead of “chairman” to convey the message that these roles are not only relegated to men. As you decide what you want to teach your kids about gender roles, be aware of the messages they get both in and out of the home.
Another important message to teach them as they grow up is that most men and women did not choose to be men or women. They grew into the role. Some boys end up with hormonal or genetic problems and end up in between – homosexuals. Some girls become lesbians. In either case, we should teach them not to discriminate or ridicule people like that. We teach them that with our comments and attitudes when we encounter them.
Answering Questions You’d Rather Avoid
A child may ask, “ Where did I come from?” Don’t give them an answer like. “a stork brought you” . You can be simple and honest in saying that “you started as a tiny egg inside Mom’s body, with Dad’s sperm, you became a baby that grew inside my uterus” Don’t say you grew in my stomach since the proper organ is the uterus.
“How come my sister needs to sit to pee and I need to stand up?” That’s because girls don’t have a penis from which urine comes out. Girls only have a small opening near the vagina called the urethra from which the urine comes out. So, it’s easier for them to urinate sitting down.
“Can boys have babies too when they grow up?” Boys, when they grow up, help to make babies since they produce the sperm which combines with a Mommy’s egg to make a baby. But only girls have a special place in her body called the uterus where the baby can grow. That’s why Daddies can never be pregnant since they don’t have a uterus.
From the time they begin to talk, children are curious to know more about their bodies and it’s functions. As parents, it is important to respond to their curiousity in a positive, open and supportive manner. Give simple and honest answers. Practice while they are young with the easier questions so when they grow up and start asking more difficult and embarrassing questions, you would have been equipped with the skill and knowhow. Sex education begins at home, and as parents, you are their first teachers.