Hysteroscopy


A hysteroscopy is a minimally invasive surgical procedure for viewing the cavity of the uterus by inserting a visualizing scope through the vagina and into the cervical opening. Hysteroscopy allows visualization of the inside of the uterus, including the openings to the Fallopian tubes, as well as direct examination of the cervix, cervical canal, and vagina. It is usually done under anesthesia in an operative set-up.
Diagnostic Hysteroscopy with Fractional D&C – this involves inserting the hysteroscope camera to view the inside of the uterus for the purpose of performing a biopsy on the lining of the uterus . This is usually done in cases of abnormal uterine bleeding or when there is a suspected mass in the uterus for biopsy.
Hysteroscopy, Polypectomy – this involves inserting the hysteroscope inside the uterus to visualize the inside cavity to locate the polyp so it may be removed by either scraping or using a hot wire.
Operative Hysteroscopy – this involves the use of an operative scope and a fluid distention media in performing the following:
- Hysteroscopic Polypectomy – use of an operative scope to resect a polyp
- Hysteroscopic Myomectomy – using an operative scope to resect myomas located inside the cavity of the uterus , called submucous myomas
- Hysteroscopic Resection of Uterine Septum – there are women with developmental abnormalities in their uterus where there may remain a septum inside the uterus , causing infertility or recurrent pregnancy loss. This septum may be resected hysteroscopically to unify the cavity of the uterus.
- Hysteroscopic Resection of Uterine Adhesions – Some women may develop intrauterine adhesions (IUA), synechia, or Asherman syndrome from obstetrical or nonobstetrical instrumentation of the uterus or infection of the urogenital tract leading to Abnormal Uterine Bleeding, Infertility, or Recurrent Pregnancy Loss. These adhesions may be removed with an Operative scope.
- Hysteroscopic Removal of Foreign Body – some women may have a retained or fragmented intrauterine device which may be removed hysteroscopically.
Open Surgery

Indications for using laparotomy over minimally invasive surgery are not hard and fast but largely depend on the experience and expertise of the surgeon, availabitlity of enabling tools or not:
- Morbidly obese patient who cannot tolerate the position of laparoscopy or robotic surgery which requires being in the “head down” or Trendelenburg position to make the bowels move out of the operative field.
- Tumor is so big that it will take hours to morcellate the specimen from the abdomen
- Massive adhesions
- Unstable patient conditions where a pneumoperitoneum (instilling carbon dioxide gas into the patient’s abdomen) would further jeopardize the patient’s condition.
- Advanced ovarian
- Lack of experienced surgeon & surgical team
- Lack of a safely functioning lap tower or robot with working instruments
Click image thumbnails to enlarge.
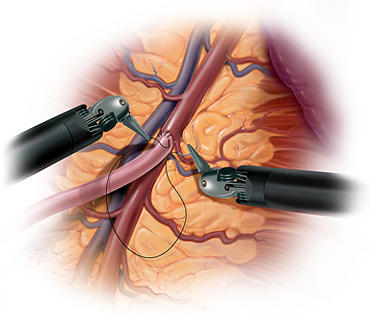
Laparoscopic Surgery


LAPAROSCOPIC SURGERY – refers to a minimally invasive surgery, also known as keyhole or band-aid surgery because the surgery is performed through tiny incisions in the abdomen through which laparoscopic instruments are inserted to accomplish the surgery. A camera, or laparoscope is inserted through the umbilicus and 2-3 other instruments ranging from 0.5-0.8cm are inserted in the abdomen at strategic locations to accomplish diagnostic procedures, management of ectopic pregnancies, removal of ovaries (laparoscopic oophorectomy or just ovarian cysts (laparoscopic oophorocystectomy), myomas (laparoscopic myomectomy) or the entire uterus (laparoscopic hysterectomy), cancer surgery. It has the advantage of minimizing downtime, rapid recovery back to activities of daily living, less chances for post op complications like pain, bleeding and infection and minimal scarring.
Robotic Surgery


ROBOTIC SURGERY – or robot-assisted surgery is a minimally invasive surgery whereby the surgeon utilizes robotic systems & platforms to allow them to perform complex procedures with more precision, accuracy and control than conventional open surgery or laparoscopic surgery. The surgical robots were designed to enhance the capabilities of open surgery such as the large incisions increasing the chances for post-op pain, wound infection & bleeding, while overcoming the limitations of laparoscopic surgery such as reverse orientation, surgeon fatigue, straight instruments with absence of rotational movements. The Da Vinci Robot was FDA approved for gynecologic surgery in 2005. Robotic surgery can be performed as an outpatient procedure or an overnight procedure, if uncomplicated. Like laparoscopic surgery, it is also a minimally invasive surgery that utilizes tiny incisions or band-aid incisions (since they are small enough to be covered with a Band-Aid). However, it is a more enabling tool, since the instruments have jointed wrist that allow it to have 7 degrees of freedom, more than the human hand and therefore seamlessly and effectively translate the surgeon’s hand movements into the more precise movements of the instrument tips. It eliminates the fulcrum effect leading to reverse orientation inherent to laparoscopic surgery. In contrast to the reverse orientation when doing laparoscopic surgery, the movements in robotic surgery are all intuitive and because the instruments rotate, it is a much easier tool for especially for suturing the defects left when removing a myoma from the uterine wall, or when suturing the vaginal stump to close it after hysterectomy.
In performing laparoscopy, usually the distance of the tissue structure from the port site on the abdomen causes amplification of motion at the instrument tip. This means that a surgeon’s tiny movement with the instruments outside the body causes a relatively large motion on the inside as seen by the camera on the monitor. This can make targeting tissues difficult and frustrating and requires a learning curve to overcome. With the daVinci Surgical Robot, motions are filtered and de-amplified up to a scale of 5 to 1. In other words, the surgeon would have to move the manipulators up to 5 inches in order to cause movement of only an inch on the inside of the body. This is even adjustable to a 3:1 ratio, meaning for every three inches of movement of the surgeon, the machine scales this down to 1 inch of movement of the instruments. This eliminates natural hand tremor entirely, allows the surgeon to target tissues with much greater ease, and gives the surgeon a certain accuracy and refinement that surpasses human capabilities for both the open and standard laparoscopic paradigms.

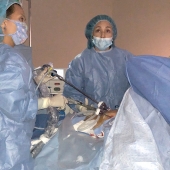
Dra. Rebecca Singson performing a robot assisted surgery.
Ergonomics is another realm of superiority for the Da Vinci robot. With traditional laparoscopic surgery, the surgeon is standing on the operating table and awkwardly struggling to move the straight instruments manually while keeping the head fixed on the monitor to visualize the movements inside the abdomen. With the Da Vinci robot, the surgeon ergonomically sits on the surgeon’s console, which memorizes the settings for every surgeon. The head is positioned with minimal strain to the neck while looking into the 3-dimensional vision system (laparoscopy only has a 2-diminsional vision system since it has only one camera whereas the robotic camera has 2 cameras: one for the left and another for the right eye). The arms are positioned to the perfect height preferred by the surgeon and the foot pedals are also adjusted to the preference of the surgeon. The vision system allows depth perception because of the 3-dimensional design and the ergonomic set up of performing surgery while seated on the surgeon’s console all translates to eliminating fatigue, especially for complicated surgeries that go on for several hours.
Open Surgery
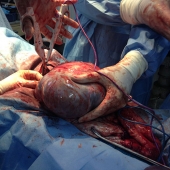
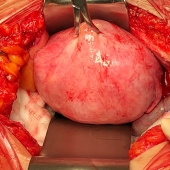
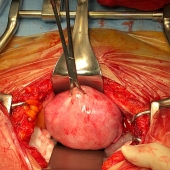
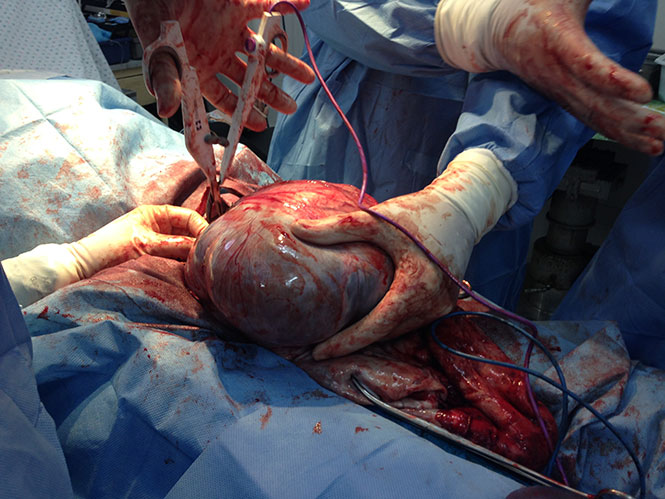
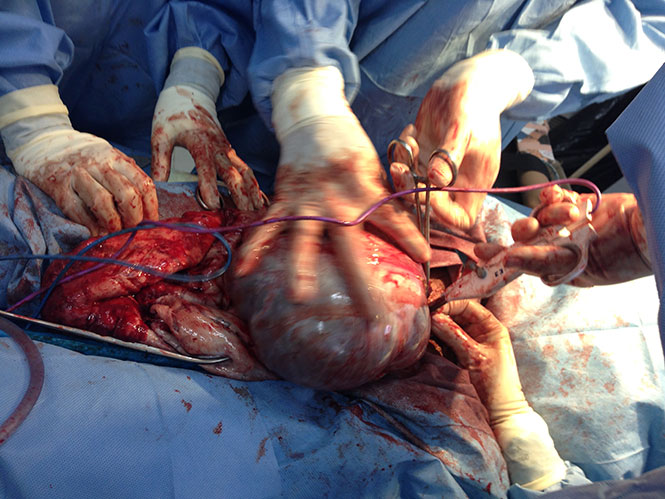
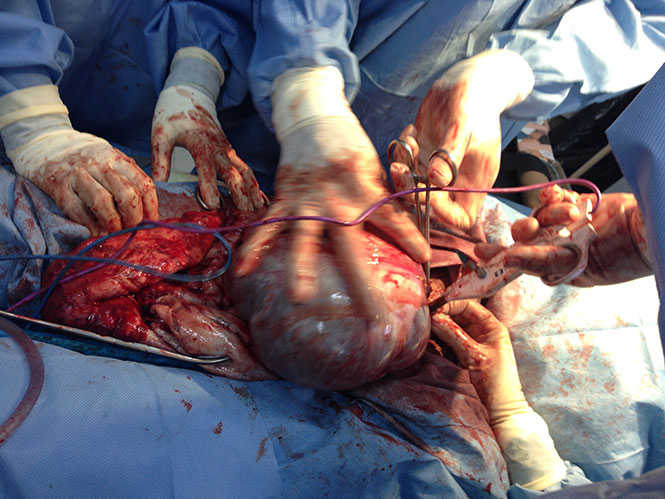
Giant Ovary


This patient is not pregnant. She had a giant ovarian tumor we removed by open surgery. Whereas, most surgeons would have cut her open with a 2-foot incision on her belly, we managed to remove this giant ovarian tumor with only a 6-inch incision, without spilling its contents inside the abdominal cavity!! Her abdomen went completely scaphoid after the giant space-occupying mass was removed l!!


Morcellated Myomata
Testimony of M.C.A.


Three years ago, I was diagnosed with a Myoma which I would monitor with an annual vaginal ultrasound.
One year ago, my Myoma suddenly grew to 7x7x6 cm and 5×54.5 cm and I was advised it was better to remove it since I would have very profuse menses, where I would consume 16 half-soaked maternity pads per day on my first two days of menses.
Since I was constantly on sick leave when I would have menses, I decided to push through with surgery. My company doctor referred me to Dra. Rebecca Singson in St. Luke’s Medical Center, Global City, who offered me a minimally invasive option.
Even if my myomas were big, I was still given a minimally invasive option. Since my company would cover a Total Laparoscopic Hysterectomy with Bilateral Salpingectomy, we proceeded to schedule that.
I underwent a Total Laparoscopic Hysterectomy with Bilateral Salpingectomy with Dra. Rebecca Singson last December 27, 2017 and was discharged the day after. I didn’t feel any significant pain and didn’t really need any pain killers. When I went home my recovery was amazingly fast and people cannot believe I actually just underwent a major surgery. I would recommend Laparoscopic Surgery for anyone needing a Hysterectomy or any other surgery in the pelvic organs.
This is the story of Miracle Baby Jana

 March 4, 2015. Please help us, the parents and medical team, storm the heavens for Jayna Marie’s life as her first day of life hangs by a thread. Her Mom, Dad and I worked for 8 solid months of infertility work-up and they miraculously got pregnant ! At 6 weeks of gestation , the baby Jayna was diagnosed on ultrasound to have Cystic Hygroma (fluid collection of the lymph at the back of the neck). While working her up for possible causes , I recommended her to Mother Remedios for spiritual healing. After a few weeks, the mass miraculously disappeared . At 26 weeks, the ultrasound showed Polyhydramnios (too much amniotic fluid ). The condition miraculously disappeared again. At 32 weeks, baby Jayna was noted to have pleural effusion on the right lung (fluid in the lungs) and beginning effusion on the left lung causing the heart to dilate . I was forced to do a C-section to try and save the baby. Luckily, baby Jayna came out crying, weighing 4.7 lbs. However, she is now intubated because she stopped breathing. On the bright side, she remains stable in her instability. Please pass this message to all prayer warriors you know because there is too much happiness to be lost for her parents (and the medical team) if we lose baby Jayna. Let us pray for this baby’s life and above all, a good quality of life, so that those who surround her may be touched and blessed by her existence. If she survives this crisis and lives, with the help of your prayers, you would be part of her endless miracles!
March 4, 2015. Please help us, the parents and medical team, storm the heavens for Jayna Marie’s life as her first day of life hangs by a thread. Her Mom, Dad and I worked for 8 solid months of infertility work-up and they miraculously got pregnant ! At 6 weeks of gestation , the baby Jayna was diagnosed on ultrasound to have Cystic Hygroma (fluid collection of the lymph at the back of the neck). While working her up for possible causes , I recommended her to Mother Remedios for spiritual healing. After a few weeks, the mass miraculously disappeared . At 26 weeks, the ultrasound showed Polyhydramnios (too much amniotic fluid ). The condition miraculously disappeared again. At 32 weeks, baby Jayna was noted to have pleural effusion on the right lung (fluid in the lungs) and beginning effusion on the left lung causing the heart to dilate . I was forced to do a C-section to try and save the baby. Luckily, baby Jayna came out crying, weighing 4.7 lbs. However, she is now intubated because she stopped breathing. On the bright side, she remains stable in her instability. Please pass this message to all prayer warriors you know because there is too much happiness to be lost for her parents (and the medical team) if we lose baby Jayna. Let us pray for this baby’s life and above all, a good quality of life, so that those who surround her may be touched and blessed by her existence. If she survives this crisis and lives, with the help of your prayers, you would be part of her endless miracles!
3/5/15
To all who prayed for Baby Jayna, consider yourselves MIRACLE WORKERS!! The baby’s water in the lungs is subsiding and I was in tears to hear that the team of neonatologists are expecting the baby to be extubated and to breath on her own IN A FEW DAYS!!! I was expecting a toxic baby that will remain intubated in the NICU for months!! They themselves were in awe that the baby is doing so well beyond their imagination!! They braced the parents that this baby will be “very sick” (they gave them the lowdown on how long the baby will stay in the Neonatal ICU, short of saying this baby can actually not make it) but Baby Jayna is incredibly improving and further stabilizing! , I can only attribute it to her guardian angels working overtime to guide the medical team and give the baby the physical support to heal her body rapidly ! Let’s continue to barrage heaven with our prayers for Baby Jayna’s ultimate recovery that her mother can finally hold her in her arms and breastfeed her like every mother and every newborn has the right to experience.
3/6/15
To all the MIRACLE WORKERS of Baby Jayna, THANK YOU!! Your prayers dramatically brought on another miracle!! She has been extubated and is breathing on her own, and the fluid in her lungs has completely disappeared!!! This has amazed and team of neonatologists because they have never expected such a rapid remarkable recovery so they are labeling this a MIRACLE!! We furthermore thought that if this baby ever makes it, we might be dealing with a chromosomal abnormality, but the geneticist said the baby doesn’t seem to fit any syndrome from her assessment!! So, let’s all please pray that she will have a normal 46 XX karyotype when the results come out and that there is no Downs, Turners or any other syndrome of chromosomal abnormality !! Her main issue now is that she is developing yellowing is the skin (jaundice) and so is currently undergoing phototherapy. Let us all pray that resolves fast so she can breastfeed from her mother’s milk.
3/7/15
More miracles to surprise your day from Baby Maria Jayna Kelsey Castro (Kelsey for the phonetic MI-RA-KEL — Kelsey). She had her first colostrum by feeding tube early morning today, so she is eating!! The neonatologist team is so awed by her progress they are hoping to wean her from her oxygen within two days!! The neonatologists want Mother Remedios, RVM (who has prayed over Baby Jayna Kelsey since her first problem was detected at 6 weeks of life) to make rounds on all their toxic babies to wield similar miracles of rapid recovery and reunion with their mothers !! Let’s continue praying for Baby Jayna Kelsey’s daily miracles. For now, the resolution of her jaundice and that her mother, so deprived of her baby, may finally cradle her for the first time since she was born.
3/10/15
The miracles continue for Baby Jayna Kelsey. She is on full feeding (36 oz every three hours!!) from her Mommy’s expressed milk ! Even God arranged for Mommy Jayne to be overflowing with milk which is fed to her baby by feeding tube !! Her oxygen is down to 2.5 liters per minute (lpm) (from 4.5 lpm 3 days ago) and they will be removing her central line in the umbilicus . Very rapidly , and against all odds, our baby has been manifesting the wonderment of our Creator and how He listens to all our prayers . Carry on, Prayer Warriors, continue to pray for Baby Jayna Kelsey to be made whole again and to finally see home with her loving parents who so miss her !!
3/18/15
Miracle update!! Baby Jayna Kelsey was moved out of the Neonatal ICU two mornings ago and has been Intermediate Care!! Isn’t it amazing how all you prayer warriors contributed to her survival ? No more oxygen , no more central venous line. Just a feeding tube for her mother milk. She is a voracious eater!! She is just to be kept under observation because she was given caffeine to make her heart beat faster. The MRI of her neck (where the Cystic Hygroma grew) is all normal and so was the 2D Echo of the heart!! Keep praying and keep the miracles coming !!
4/1/15
Our miracle Baby Jayna Kelsey is now home since yesterday with Mom and Dad. The family wants to express their heartfelt thanks for all your prayers, the sum total of which led to the this big MIRACLE OF LIFE called Jayna Kelsey!!
4/15/16
Remember Baby Jayna Kelsey, our miracle baby, for whom we spent countless nights praying that she would pull through, is now turning 1 year old !! Thanks to all your prayers she is a normal, active, vibrant baby girl!
Medicine to shrink myomas


NEW DRUG TO SHRINK MYOMAS. The growth of myomas or fibroids have been found to be promoted by progesterone. Therefore blocking the progesterone receptors have been found to reduce myomas as has been proven by a new drug called ULIPRISTAL (brand name Esmya), available in the Philippines. It has contraceptive benefits and is particularly effective for stopping the bleeding caused by myomas . However , it is contraindicated in patients, especially those in the perimenopausal or menopausal stage where cancer might be suspected . In patients with huge or multiple myomas beyond 8 cm, a hysterectomy can still be done minimally invasively via robotic surgery. Because the instruments of Robotic surgery have 7 degrees of movement, which surpasses the human hand, suturing is made far more easily than laparoscopic surgery . Blood loss is less than open surgery and downtime is reduced markedly from 6 weeks in an open surgery to one week with a robotic surgery . Before subjecting yourself to an open surgery examine your options and consult with a Gynecologist who performs robotic surgery so see if it is for you.