Robotic Surgery – Step by Step

Step 1: Applying the Trocars on the abdomen
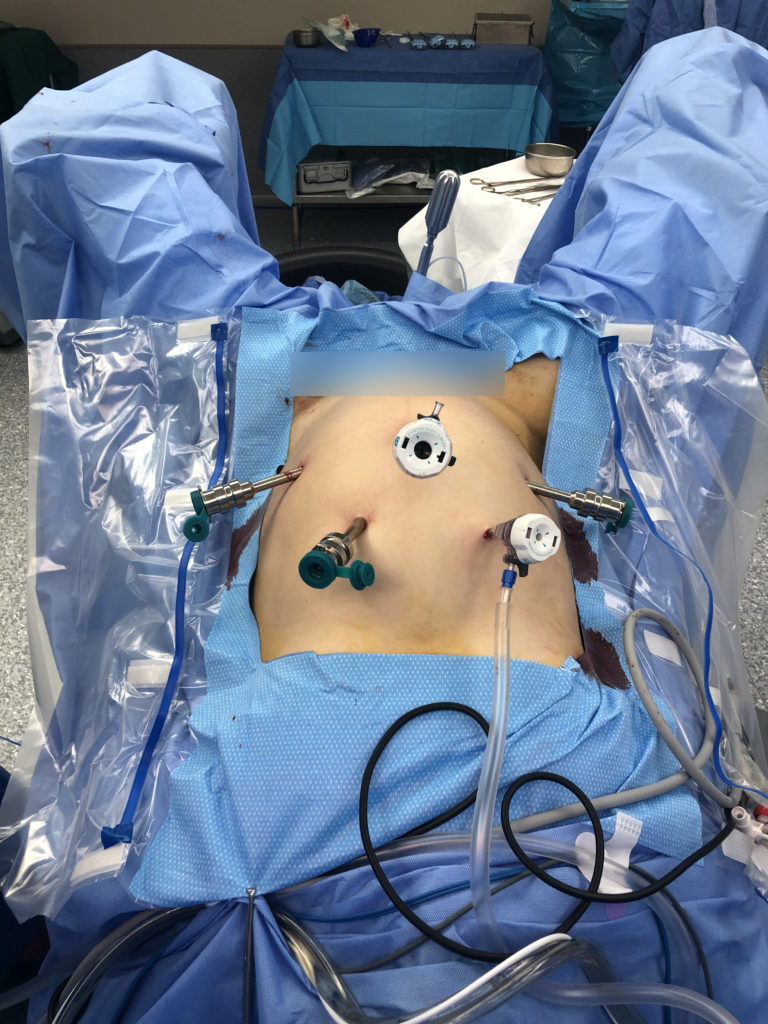
Step 2: Docking the robot to the ports
Step 3: Attach the camera and the instruments
SURROGACY : HOPE FOR THE HOPELESS?

Karina has been married for 20 years. At 20, she was diagnosed with severe endometriosis for which she has undergone two surgeries to remove the cysts in her ovaries. Her infertility has been a source of frustration until at age 42, she learned of surrogacy. She flew to the United States with her husband to find a surrogate mom. By artificial insemination, her husband’s sperm was inseminated to the surrogate woman, resulting in a live baby girl they eventually brought back to the Philippines.
Surrogacy is an arrangement whereby a woman, called the surrogate, agrees to carry the child of another woman, with the agreement that the surrogate will surrender the child upon birth to the mom who commissioned the child, and the surrogate relinquishes all her parental rights over the child,.
There are two general types of surrogacy:
Traditional surrogacy – the intended father impregnates the surrogate mom using her own ova or eggs and the pregnancy is carried in her womb.
Gestational surrogacy – the sperm of the intended father and the eggs of the intended mother are fertilized outside the womb and the resulting fertilized zygote or blastocyst is placed into the womb of the surrogate who carries the pregnancy.
REASONS FOR SURROGACY – the woman may be infertile or unable to carry a pregnancy to term for various reasons:
- INABILITY TO OVULATE:
- Some women may have Polycystic Ovary Syndrome that prevents them from releasing eggs and ovulating.
- Others may have Premature Ovarian Failure, a condition the ovary stops functioning even before the age of 40 years old. This can happen after exposure to toxic agents like radiation, chemotherapy or heavy metals.
- Ovarian cysts like endometriosis can damage the normal ovarian tissue especially if they occur on both ovaries. This condition also causes inflammatory condition and distortion of the anatomy along with adhesions, thus, preventing the sperm from meeting the egg or preventing implantation.
- IMMUNOLOGIC PROBLEMS – some women have Immunologic Disease of Pregnancy, a condition that predisposes patients to clotting or thrombosis, thereby cutting off the supply to the fetus during pregnancy, causing recurrent miscarriages, intrauterine fetal death, premature labor and hypertension.
- UTERINE ABNORMALITIES /PROBLEMS
- 1 in 4500 women can develop a congenital malformation resulting in a missing uterus and variable degrees of underdevelopment of the vagina. This is called the Mullerian Agenesis or Mayer-Rokitansky-Kuster-Hauser Syndrome.
- Bicornuate uterus-
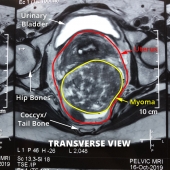
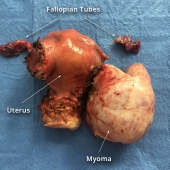
- Some women may also have multiple myomata which may cause major distortion of the cavity of the uterus preventing implantation or causing recurrent miscarriages.
- Adenomyosis is also another condition that can prevent pregnancy since the lining of the uterus implants on the muscle of the uterus, causing a thickening and hardening of the muscle of the uterus.
- Surgical absence of the uterus- Some women may have had to undergo a hysterectomy for uterine or cervical or ovarian cancer, or for intractable abnormal uterine bleeding due to tumors.
- MEDICAL CONDITIONS – the woman may have a valvular heart disease, kidney disease or severe hypertension or diabetes that can worsen with pregnancy, jeopardize the fetus and cause prematurity or demise. A history of cancer or leukemia that requires the patient to be on maintenance meds contraindicating pregnancy can also be a deterrent to pregnancy.
- AGE – some women decide too late in life that they want babies because the demands of career were prioritized. Or, by the time they found the right partner or another partner they wanted to have children with, it was beyond 42-45 years of age. Most IVF clinics cut off at 42-45 years beyond which they will not accept patients for fertility treatments.
- GAY COUPLES – same sex partners will obviously need help to conceive. Male-male partners will require an egg donor and a surrogate mother to carry the pregnancy. Female-female partners will simply require a donor because usually one or the other will be willing to carry the pregnancy.
SURROGACY IN THE PHILIPPINES
Currently, there is no law prohibiting or openly allowing surrogacy. A bill prohibiting surrogacy was filed by Sen. Manny Villar on June 7, 2006. However, it did not gain support and was, therefore, never passed. No one has proposed any similar bill since.
The Philippines Society of Reproductive Medicine in 2006 and the Philippine Obstetrical and Gynecological Society in 2011 made a stand that it is unethical for a third party be involved in a couple trying to conceive. This means that donor eggs, donor sperm and surrogacy are not practiced by licensed fertility experts and is deemed unethical.
HOW TO CHOOSE A SURROGATE?
Commercial surrogacy, where the mother is paid a fee, is allowed in some states in the US, India, Russia and Ukraine. In Denmark, U.K, Belgium, Ireland, and, Hong Kong, surrogacy is allowed as long as the mother is not paid. France, Germany, Italy, Spain, Portugal, Bulgaria, Thailand and Cambodia prohibit all forms of surrogacy.
In choosing a surrogate mother, the following criteria are recommended:
-She must be at least 21 years old.
-She must at least have given birth previously to a child as proof of fertility and to insure that she understand what is involved with childbearing.
-Must be mentally sound and evaluated and counselled by a professional on mental health to insure she will not have issues on giving up the child.
-Must be willing to sign a contract that she is going to perform her role in insuring a healthy pregnancy, follow a diet, supplementation and go for regular pre-natal check-ups. Above all, she must sign that she is willing to give up the baby and all parental rights after the baby is born.
ADVANTAGES OF SURROGACY
- It allows a couple to create a family. There is a growing number of LGBT couples who are desirous of having children to complete their family. Women who lost their uterus to cancer or have medical illnesses or have passed the age of fertility can hope to have children.
- The expectations are defined. In cases where there is a legally binding contract, the rights of the surrogate mother are defined and the intended parents are also protected by law.
- There is a high chance of success. Because the surrogate has a history of a previous healthy birth, the chances are higher for the surrogate to carry a pregnancy than through fertility treatments.
DISADVANTAGES OF SURROGACY:
- It is not simple. One has to deal with complex medical procedures as well as legal paperwork
- It can be emotionally taxing to the surrogate mom. Many of them are detached from their families for the duration of their pregnancy to insure they will be properly nourished and cared for and giving psychological support. It still results in depression for many to know they cannot be a mother to the baby they are carrying. There are cases when the mother opts to keep the child and that can cause emotional and legal battles with the intending parents.
- It can be costly. The intending parents have to pay for the surrogate mom, her food, living expenses, supplements and medical fees for the procedures as well as the agency, if one is involved.
HOW MUCH DOES IT COST?
The cost varies from country to country. This is an approximate cost for the various countries according to Families Through Surrogacy:
- US – $100,000 (£60,000)
- India – $47,350
- Thailand – $52,000
- Ukraine – $49,950
- Georgia – $49,950
- Mexico – $45,000
There is hope for childless parents who have not been blessed with children naturally to still have their own child through surrogacy. The advancement of science has made possible the technology. The challenge is how to keep the practice from being abused by laying down the legal, moral and eithical ground rules to make it more acceptable to more countries to allow.
CS Hysterectomy for Placenta Previa Percreta
Chef Luigi Muhlach
January 19 at 7:36 PM
Through our struggles in life, we grow spiritually. When we are able to experience first- hand how emotionally unstable and weak we can become and how desperately we need HIM. When circumstances teach you that the most important relationship you’ll ever have is the one you have with God.
patty was diagnosed with placenta percreta last october. It is the rarest and most severe form of placenta accreta and is a life threatening condition. It occurs when the placenta attaches too deeply into the uterine wall. In patty’s case, it was already starting to attach to her bladder. Mortality rate is as high as 9.5% and 24% for mother and child when placenta percreta is complicated by bladder invasion.
The operation was very complicated. We had two obgynes and a urologist in the operating room. It took the doctors 4 hours. patty lost 8 units of blood and used up all 10 units we had on standby for her and we had to spend money we did not even have.
Less than 2 weeks after being discharged, patty was back in the hospital. We discovered that she didnt heal well and developed pools of abscess that caused her severe back pain and stomach ache. She had to go back to the operating room for an aspiration.
It was a very traumatic experience for us but we were able to pull through.
Challenges cause us to stretch our faith, to seek God more than ever, To get to know him more and to be hungry for his presence.
This experience has brought me and patty closer to god and to each other. This has made us stronger as individuals and as a team. It has taught us that it is possible to go through the toughest storms in life peacefully, confidently and gracefully when you know who God is, that when you are going through trials and nothing makes sense, we can rest knowing that he loves us and has our best interest in mind.
Source: https://www.facebook.com/muhlachluigi/videos/980443099010192/
Ovarian Cysts, What are They?


What are ovarian cysts? — Anatomically, a woman’s reproductive organs are composed of a uterus, a left and right Fallopian tube attached to the uterus and a left and right ovary underneath the Fallopian tubes. Sometimes, fluid can fill up a growth within an ovary creating an ovarian cyst. In women who are having their monthly period, the ovaries release an egg about once a month. In women over 40 years old who learn they have ovarian cysts, the first concern is the possibility for cancer although in reality, worry about cancer when they learn they have cysts. But most of the time, cysts are not cancer.
How frequently do we find ovarian cysts in women?
Simple cysts are filled with fluid. Monthly ovulation will often include the formation of cysts, and they are not usually a cause for concern. When they cause no problems, they are called functional cysts.
Complex cysts are less common than simple cysts. Either blood or a hard substance fills complex cysts. Unlike simple cysts, complex cysts are not related to the typical menstrual cycle.
The reported prevalence of ovarian cysts in women is between 8% and 18% of women although not all ovarian cysts need surgery . 1
In the U.S., only 5% to 10% of women undergo surgery for ovarian cysts in their lifetime and only 13% to 21% of these cysts are malignant.2
What causes ovarian cysts? — There are many possible causes of ovarian cysts. The most common causes of simple cysts include:
- Ovulation – Ovulation is when an egg is released from the ovary each month. For this to happen, the ovary grows a sac, called a “follicle.” Sometimes, a follicle grows but does not release an egg and instead forms a cyst.
Corpus Luteum Cyst – if a woman gets pregnant after the egg is released, a cyst can stay on the ovary for weeks or months. It is formed on the ovary at the site of a follicle, or sac, that has matured and released its ovum or egg, in the process known as ovulation. The corpus luteum is made up of lutein cells (from the Latin luteus, meaning “saffron-yellow”), which develop immediately following ovulation, when yellow pigment and lipids accumulate within the granulosa cells lining the follicle. It may, however, fill with fluid or blood, causing the corpus luteum to expand into a cyst, and stay in the ovary. These kinds of cysts are not harmful and usually go away on their own especially if the patient is not pregnant. It may persist in pregnancy to produce progesterone and support the pregnancy until the placenta takes over the production of Progesterone to support the pregnancy.
Hemorrhagic Corpus Luteum Cyst – this is an ovarian cyst that develops because of occurrence of bleeding into a follicle or corpus luteum.3
Polycystic ovary syndrome (also called PCOS) – In women with this condition, the ovary grows many small cysts, instead of 1 big follicle that goes away each month. These cysts usually do not go away, but the cysts themselves do not need to be treated or removed. Treatment is mainly medical to address the insulin resistant problem and anovulation.
The different types of Complex Ovarian cysts are the ff:
Dermoid cysts – These are a common type of cyst. They sometimes have teeth, hair, or fat in them. That might sound strange. Dermoid cysts are normally not harmful to your health, but your doctor might want to remove them with surgery.
Hemorrhagic Corpus Luteum Cyst – this is an ovarian cyst that develops because of occurrence of bleeding into a follicle or corpus luteum.3,4
Cystadenomas.These cysts are made of ovarian tissue and contain mucus, called mucinous cystadenomas or serous fluid called serous cystadenomas.
Endometriosis – Endometriosis is a condition where tissue normally found in the lining of woman’s uterus called endometrium, implants outside of the uterus, like in the ovaries, the back or the front of the uterus or anywhere in the abdominal cavity, producing endometriotic implants. Thus, when a woman bleeds during menstruation, she also bleeds into those implants outside the uterus causing pelvic pain during their periods or at other times, pain in the belly during sex, or trouble getting pregnant. Endometriotic cysts in the ovary are filled with blood that look like chocolate syrup. Hence, they are also called “chocolate cysts”.
Ovarian Cancer – Cancer is the cause of ovarian cysts in less than 1 in 100 cases. Ovarian cancer is most likely to affect older women who have been through menopause (no longer have a monthly period) or who have a family history of ovarian cancer. This “silent” cancer is most often discovered and treated when it has already spread, contributing to a reported 5-year survival rate of only 33% to 46%.5-7 Ideally, ovarian cancer would be found and removed while still confined to the ovary, when the 5-year survival rate is greater than 90%.
Unfortunately, there does not seem to be a precursor lesion for most ovarian cancers, and there is no good way of finding it in the stage 1 phase, so detecting this cancer before it spreads remains an elusive goal.5,8
What are the symptoms of ovarian cysts? — Many women have no symptoms. Sometimes, they are only discovered on routine physical exam or ultrasound.
The usual symptoms are the following:
- pressure or bloating in the abdomen
- general pain or right or left pain in the lower abdomen
- abnormal vaginal bleeding
- vomiting or nausea or pain if the ovarian cyst or twists
- frequency or urgency of urination if the cyst pushes on the bladder
- a sudden, severe, unbearable stabbing pain if the cyst ruptures, prompting emergency room consult
In the case of endometriomas, a patient may have the following additional symptoms that may include: - constipation
- diarrhea
- painful intercourse (called dyspareunia)
- nausea
- pain during periods (called dysmenorrhea)
- fertility problems
- pain during bowel movements (called dyschezia)
Immediate consult should be made if you experience severe pain in the abdomen, fever and vomiting.
How do we test for ovarian cysts?
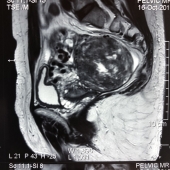
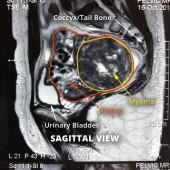
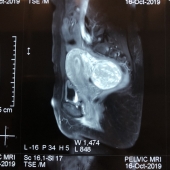
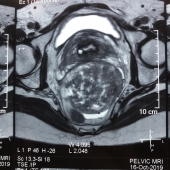
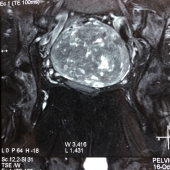
Imaging tests – The most common kind is a pelvic, vaginal or transrectal (it still a virgin) ultrasound. This test uses sound waves to create a picture of your uterus and ovaries, map out the location, size and if it is attached or adherent to the uterus or intestines. An Ultrasound with a Doppler can map out the flow in the blood vessels to differentiate a benign from a malignant tumor. An MRI or a CT scan may also be ordered and correlated with the findings on ultrasound.
Blood tests to check for pregnancy or check for elevation of certain tumor markers like CA-125, CEA, HE-14, BHCG, which may raise the suspicion of cancer.
How are ovarian cysts treated? — Treatment depends on the type of cyst and what your symptoms are. Possible treatments include:
Watchful Waiting – The cyst may be simply observed, if small and asymptomatic with an ultrasound every couple of months. Your cysts might stay the same size, get smaller, or even go away. In those cases, you usually don’t need to do anything to treat them.
Birth control pills and other types of hormone-like pills – This medicine can stop some types of new cysts from growing and may even shrink some endometriomas
Surgery to remove a cyst is called Oophorocystectomy while removal of the whole ovary is called Oophorectomy. The type of surgery will depend on the size of the tumor, as well as desire for fertility. Cysts up to 5 cm in size may be removed laparoscopically, depending on the surgeon’s skill and experience. Larger cysts may be removed by open surgery or minimally invasively by Robotic Surgery .
- Greenlee RT, Kessel B, Williams CR, et al. Prevalence, incidence, and natural history of simple ovarian cysts among women >55 years old in a large cancer screening trial. Am J Obstet Gynecol 2010; 202:373.e1-e9
- NIH Consensus Development Panel on Ovarian Cancer. NIH consensus conference. Ovarian cancer. Screening, treatment, and follow-up. JAMA 1995; 273:491–497
- N. Yoffe, M. Bronshtein, J. Brandes, Z. Blumenfeld. Hemorrhagic ovarian cyst detection by transvaginal sonography: the great imitator. Gynecol Endocrinol, 5 (1991), pp. 123-129
- Jain KA. Sonographic spectrum of hemorrhagic ovarian cysts. J Ultrasound Med 2002; 21:879–886.
- Clarke-Pearson DL. Clinical practice. Screening for ovarian cancer. N Engl J Med 2009; 361:170–177.
- National Cancer Institute. Surveillance Epidemiology and End Results (SEER). Cancer statistics on ovarian cancer. http://seer.cancer.gov/statfacts/html/ovary.html. Accessed May 9, 2013.
- American Cancer Society. Survival by ovarian cancer stage. www.cancer.org/Cancer/OvarianCancer/DetailedGuide/ovarian-cancer-survival-rates. Accessed May 9, 2013.
- Brown PO, Palmer C. The preclinical natural history of serous ovarian cancer: defining the target for early detection. PLoS Med 2009; 6:e1000114